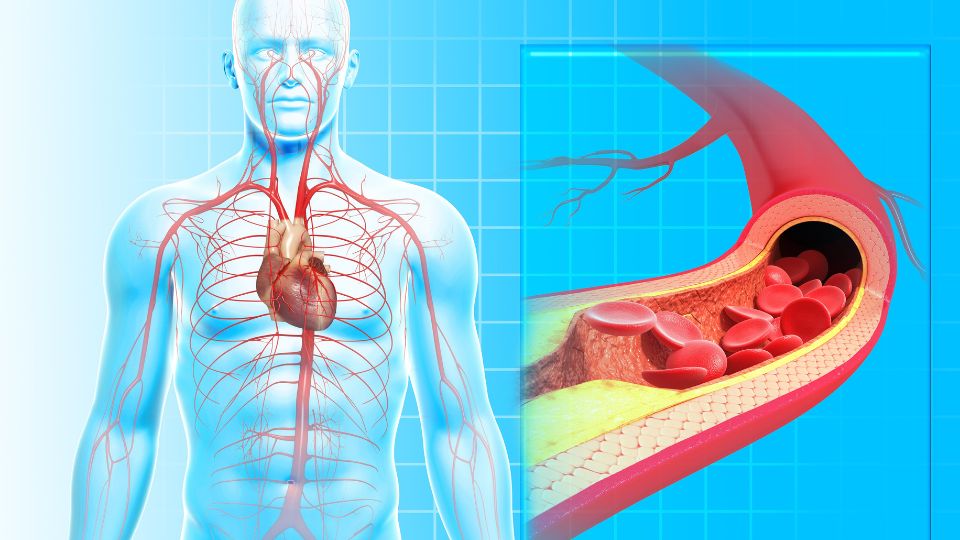
Your entire body relies on your arteries, the blood vessels that carry oxygen-rich blood to every part of your body. These vessels do their important work round the clock, unnoticed, but when there is a blockage, things can go dangerously wrong. Atherosclerosis is the accumulation of fat and other material in the arteries. If allowed to continue long enough, it can cause dangerous health problems, including heart attack and stroke. Atherosclerosis becomes more likely to develop as you age, but it isn’t inevitable. Keep reading to find out what contributes to the development of atherosclerosis, what it can do to your body, and it can be treated and prevented.
What Is Atherosclerosis?
Atherosclerosis is the process where the arteries of the body become narrowed due to a buildup of fatty plaque. As the blockage continues to grow, atherosclerosis gradually restricts the blood supply to the body’s organs and tissues. Arteries carry freshly-oxygenated blood from the heart to the rest of the body, and atherosclerosis can cause various problems depending on where the blockage occurs.
What Is The Difference Between Arteriosclerosis And Atherosclerosis?
Arteriosclerosis is when the arteries become thicker and less flexible. Atherosclerosis is a type of arteriosclerosis caused by fatty plaque building up in the arteries.
What Does The Plaque Do In The Arteries?
Once the plaque is inside the arteries, there are three things that could happen. Firstly, plaque may grow to a certain size and then stop. If the blood flow isn’t obstructed, there may never be symptoms. Secondly, it may grow slowly and eventually cause serious blockages. The type of damage this causes depends on where in the body the blockage is. Thirdly, it may rupture suddenly, causing a blood clot inside an artery. Depending on where this occurs, the result can be a stroke or a heart attack.
The kind of plaques that rupture are called unstable plaques, or vulnerable plaques. Those at a lower risk of rupture are known as stable plaques.
What Causes Atherosclerosis?
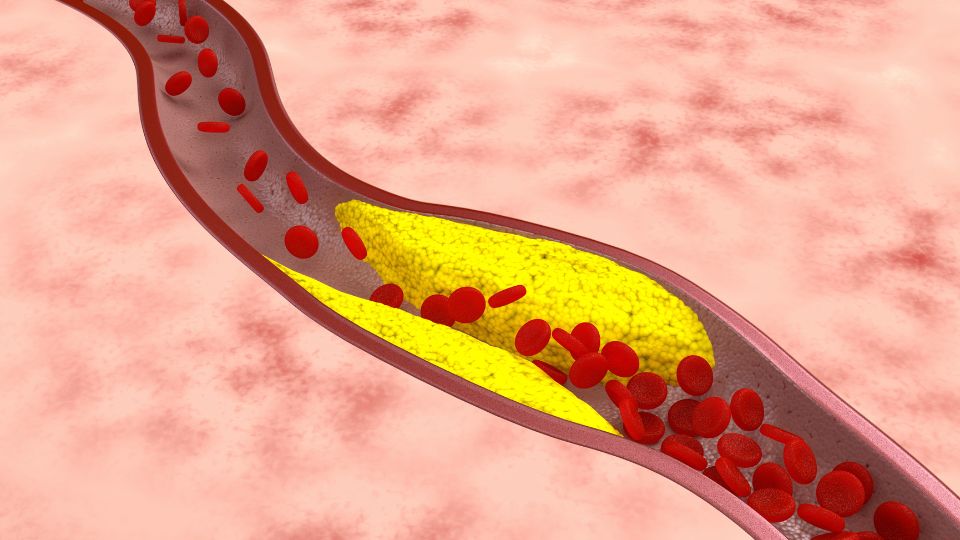
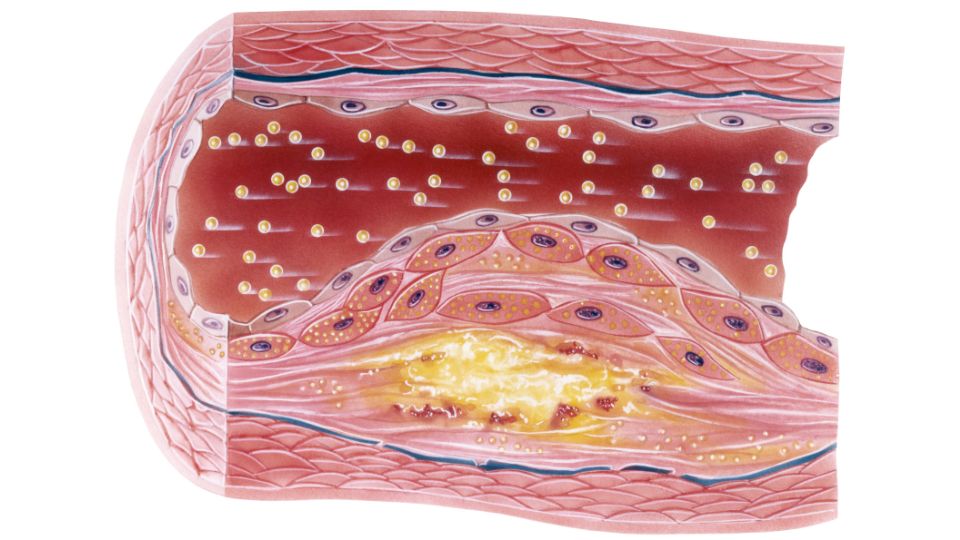
Arteries are blood vessels that carry freshly-oxygenated blood all over the body. Every artery is lined with a thin layer of cells called the endothelium. Atherosclerosis begins when the endothelium is damaged. This makes LDL cholesterol (‘bad’ cholesterol) stick to the damaged part of the artery’s inner wall. This process triggers an immune response, and white blood cells come to the site to clean up the damage but cause inflammation. This mixture of cell material, cholesterol and other substances continues to build up in the artery and may cause a blockage. Such a blockage can result in constriction of blood flow, or, if a piece of the plaque ruptures, a blood clot. Either can be life-threatening, causing life-threatening medical issues like stroke and heart attack and requiring immediate first aid.
What Is Arterial Plaque Made Of?
Also called atheroma, arterial plaque is made of substances including cholesterol and other fats, calcium and cellular waste products.
What Are The 4 Stages Of Atherosclerosis?
The development of atherosclerosis can be divided into four stages:
- The endothelium is damaged: this can be caused by factors including high blood pressure, obesity, high cholesterol levels, smoking and inflammatory diseases. This damage causes white blood cells to flock to the area, resulting in inflammation.
- A fatty streak forms: when white blood cells consume too much LDL cholesterol in their efforts to clean up damage in the artery, they become foam cells (this name comes from their foamy appearance. The yellow streak formed by these foam cells is the first visible indication of atherosclerosis.
- Fibrofatty plaque develops: material, including dead foam cells, accumulates over the fatty streak, and the plaque becomes larger. A fibrous cap of connective tissue develops over the top of the plaque to stop pieces of it from breaking off and floating away in the bloodstream. The continued growth of the plaque makes it increasingly hard for blood to get through the artery.
- Plaque ruptures: the fibrous cap is the body’s protective measure to stop the plaque from breaking up, but this cap can break. When this happens, a blood clot forms over the top of the opening that’s left. This clot blocks blood flow; if it is dislodged and travels away in the bloodstream, it can cause serious problems, including stroke.
Where Can You Get Atherosclerosis?
Atherosclerosis can develop in any artery in the body, and it has different names depending on where it occurs.
Carotid Artery Disease
Carotid artery disease is the accumulation of plaque in the walls of the carotid arteries, which supply the brain with 80% of its required blood and provide blood to the face and neck. Carotid artery disease is sometimes called carotid artery stenosis (narrowing).
Vertebral Artery Disease
The vertebral arteries provide the other 20% of the brain’s blood supply, connecting to the back of the brain, including the brainstem and cerebellum. They also supply blood to the spinal cord. Plaque buildup in these arteries is called vertebral artery disease or vertebral artery stenosis.
Coronary Artery Disease
Coronary artery disease (CAD) is a buildup of plaque in the arteries that provide blood to the heart.
Mesenteric Artery Ischaemia
Mesenteric artery ischaemia is the accumulation of plaque in the arteries supplying blood to the small and large intestines.
Renal Artery Disease
Also called renal artery stenosis, renal artery disease is atherosclerosis in the arteries that carry blood to the kidneys.
Peripheral Artery Disease
Peripheral artery disease (PAD, also called peripheral arterial disease) is the growth of plaque in the arteries that take blood from the heart to the other parts of the body and is most commonly experienced in the legs.
What Are The Symptoms Of Atherosclerosis?
The symptoms of atherosclerosis differ depending on where the arterial plaque is in the body and how much of the blood flow is blocked.
| Location Of Atherosclerosis In The Body | Symptom |
| Heart and coronary arteries |
The first symptom may be a heart attack:
If you experience the symptoms of a heart attack, seek medical help immediately |
| Brain and arteries leading to the brain |
The first symptom may be a stroke or a TIA (a ‘mini stroke’, which has similar symptoms):
If you experience the symptoms of stroke, seek medical help immediately |
| Arms and legs | Symptoms of PAD:
|
| Arteries leading to kidneys |
|
| Arteries supplying small and large intestines |
|
Serious health problems like a heart attack or stroke can sometimes be the first sign of atherosclerosis. To be as well-prepared as you can for any event, consider enrolling in a first aid course.
What Are The Risk Factors For Atherosclerosis?
Some risk factors for atherosclerosis are avoidable, and some aren’t. Either way, it’s a good idea to be aware of them.
High Blood Pressure
High blood pressure increases the level of force of the blood against the artery walls, damaging them and leading to further buildup of plaque.
High Levels Of Cholesterol And Triglycerides
High cholesterol levels in the blood provide the fatty material that makes up most of the substance of arterial plaque.
Diabetes
Long-term high blood sugar (hyperglycaemia), such as that which occurs with poorly-controlled diabetes, creates a cellular environment that speeds up the process of atherosclerosis.
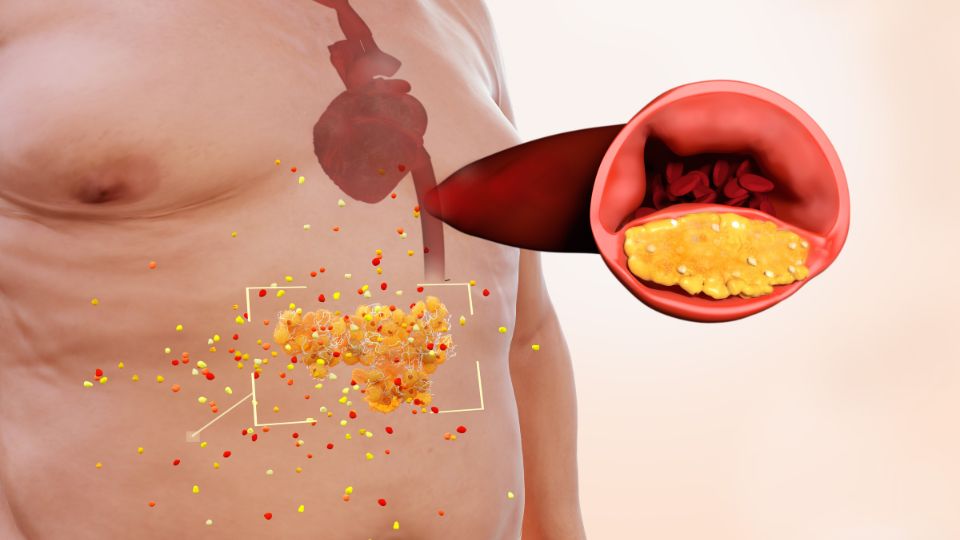
Obesity
Obesity causes inflammation, which aids the development of atherosclerosis.
Sleep Apnoea
The buildup of arterial plaque may be accelerated in people with untreated sleep apnoea.
Physical Inactivity
Regular exercise helps improve many of the risk factors associated with atherosclerosis, including blood pressure, weight and cholesterol levels. Italian researchers found that the effects of ageing are less damaging to the endothelial cells in people who exercise, and endothelial damage is the first step in the development of atherosclerosis.
Smoking
The toxic chemicals in cigarette smoke cause inflammation in the blood vessels and contribute to the development of plaque.
Metabolic Syndrome
Metabolic syndrome is a collection of conditions found together, including high cholesterol or triglyceride levels, high blood pressure, high blood sugar, and central obesity (body fat around the waist) that create a problematic state of inflammation in the body that makes it easier for atherosclerosis to develop.
Unhealthy Diet
A diet high in saturated fat can elevate cholesterol levels, providing more material for the growth of plaque. A diet high in salt can elevate your blood pressure and cause damage to the walls of your arteries, accelerating the development of atherosclerosis.
Family History
A family history of heart disease early in life (a diagnosis before the age of 45 in men and before 55 in women) can increase your risk of atherosclerosis, as can the presence of certain genes, such as those responsible for familial hypercholesterolaemia.
Inflammatory Diseases
As inflammation inside the arteries is an important part of the development of atherosclerosis, it should come as no surprise that inflammatory diseases like lupus, arthritis or psoriasis can increase your risk.
Age
Some health conditions are more common in younger people, and some are more common in older people, and the incidence of atherosclerosis definitely goes up with age. The development of arterial plaque gathers speed between the ages of 40 and 50, with one study finding that 40% of people within this age range ‘showed major progression of atherosclerosis‘.
Risk Factors Specifically Affecting Women:
- Polycystic ovary syndrome is a hormonal condition that causes symptoms including cysts on the ovaries
- A history of gestational diabetes, diabetes that begins during pregnancy
- A history of preeclampsia, high blood pressure during pregnancy
- Having had a hysterectomy and oophorectomy surgery (removal of the uterus and ovaries).
- Endometriosis, a disorder where the uterine lining grows outside of the uterus, is associated with a higher risk of coronary heart disease (atherosclerosis in the coronary arteries), although there is a possibility this may be partly due to the greater likelihood of women with endometriosis getting hysterectomy and oophorectomy surgery
What Are The Complications Of Atherosclerosis?
Atherosclerosis can cause serious complications anywhere in the body.
Brain
Atherosclerosis in the arteries inside or leading to the brain can result in a transient ischaemic attack (or TIA, also known as a mini-stroke) or a stroke. Stroke can also occur when a blood clot develops elsewhere in the body and travels to the brain in the bloodstream, which is more common in people with atherosclerosis. Finally, deprivation of blood supply to the brain can gradually lead to vascular dementia.
Heart
Coronary heart disease, or plaque build-up in the coronary arteries that transport blood to the heart, can cause and contribute to life-threatening heart problems, including arrhythmia, aortic aneurysm, heart failure, heart attack and cardiac arrest. Many of these heart problems can occur without warning. To be prepared for any scenario, enrol in an accredited first aid course.
Organs
Atherosclerosis in the renal arteries (renal artery disease or renal artery stenosis) can cause high blood pressure, chronic kidney disease and kidney failure. Mesenteric artery ischaemia (atherosclerosis in the arteries leading to the intestines) can cause sepsis or bowel tissue death, both potentially fatal.
Limbs
Peripheral artery disease can cause critical limb ischaemia, an inadequate long-term supply of blood to the limbs, which can, in turn, eventually result in gangrene and limb loss.
Everywhere
Atherosclerosis can cause aneurysms. An aneurysm is a bulging, weakened artery or vein that can rupture with life-threatening results. An aneurysm can occur anywhere in the body.
How Is Atherosclerosis Diagnosed
Below is a list of techniques your doctor may use to help diagnose atherosclerosis, ranging from basic to complex.
Blood Tests
To check for atherosclerosis, your doctor may conduct blood tests to evaluate your blood cholesterol and blood sugar levels. There may also be a test for c-reactive protein, a substance whose presence in the body can indicate inflammation.
Blood Pressure
Your blood pressure may be tested because high blood pressure is a risk factor for atherosclerosis.
Tests For Obesity
Your doctor may take your waist measurements and calculate your body mass index to determine whether you are overweight.
Electrocardiogram
A doctor may use an electrocardiogram (ECG, sometimes called EKG in reference to the German spelling) to look for signs of cardiovascular disease. An ECG is a non-invasive and painless test in which wires are attached to your chest using sticky pads to generate a recording of your heart rhythm. An ECG can’t specifically detect atherosclerosis, but it can detect irregularities in your heartbeat that may indicate coronary artery disease.
Heart Imaging Tests
Heart imaging tests can be used to create pictures of your heart and the surrounding blood vessels.
Coronary Angiography
A coronary angiogram is a test where a thin catheter is inserted into an artery in your groin or wrist that is connected to your heart. Dye is injected into the bloodstream through the catheter so an x-ray can more effectively pick up images of blocked arteries.
Cardiac Magnetic Resonance Imaging (MRI)
Magnetic resonance imaging (MRI) is a technique where magnets and radio waves are used to create cross-sectional images of the inside of your body. These cross-sections can then be stacked to create a three-dimensional image. A cardiac MRI can be used to detect damage to tissue or problems with blood flow. An MRI does not use radiation.
Cardiac Positron Emission Tomography (PET) Scanning
Positron emission tomography (PET) scanning is an imaging technique where a small amount of radioactive material called a ‘tracer’ is injected into your body to help create images with a large scanner that your whole body can slide into as you lie on a moveable table. The tracer is more readily absorbed by damaged tissues, helping to create a more detailed picture of problem areas.
Coronary Computed Tomographic (CT) Angiography
In a Coronary Computed Tomographic (CT) Angiogram, a picture of the heart and blood vessels is taken using a powerful x-ray machine that your whole body goes inside. One advantage it has over a regular coronary angiogram is that there is no catheter inserted – it is non-invasive. A disadvantage is that, like a PET scan, radiation is involved, so it cannot be used for some people, including pregnant women.
Coronary Calcium Scan
A coronary calcium scan is a special x-ray of your heart that can be used to determine if there is plaque buildup in the walls of your coronary arteries (plaque contains calcium). Like a CT angiogram and a PET scan, a coronary calcium scan involves lying on a moveable table that slides into a large tube-like machine. Like both, it involves some radiation exposure.
Stress Tests
During a stress test, your doctor monitors your heart’s functioning under physical stress, either by having you exercise with a treadmill or a stationary bike or by giving you medication that forces your heart to beat faster. This is done with you attached to an ECG and wearing a cuff around your arm to gauge your blood pressure. There is also a variation called a nuclear stress test where you perform the exercise as normal but have a nuclear tracer injected and undergo a PET scan before and after exercise.
Ankle-Brachial Index (ABI) Test
In an ankle-brachial index (ABI) test, a doctor measures the blood pressure in both of your arms and both of your ankles. If there is found to be insufficient blood flow in your legs compared with your arms, this can indicate peripheral artery disease, although more tests may be done.
How Is Atherosclerosis Treated?
Depending on how advanced the buildup of plaque is and how large and problematic any blockages are, atherosclerosis may be treated with approaches including lifestyle changes, medications, and surgical procedures.

Lifestyle Changes
Eat A Healthy Diet
A diet high in vegetables, fruits and whole grains and low in processed carbohydrates (like white bread), saturated fats, salt and sugar can help to stop the development of atherosclerosis and a host of other health problems, including type 2 diabetes, fatty liver and some cancers.
Get Regular Exercise
Regular exercise has multiple benefits for your health, including lowering the risk of obesity, diabetes and other conditions that promote the development of atherosclerosis. More directly, exercise enhances the health of your arteries by improving blood flow and reducing blood pressure. Adults should aim to get some exercise most days of the week. A good goal to work towards is 150 minutes of moderate aerobic exercise or 75 minutes of vigorous aerobic exercise every week, plus two or more days each week of ‘muscle-strengthening activities’ that work all of the body’s main muscle groups — this can include any form of exercise that uses weights or your body weight for resistance.
Control Your Weight
Your risk of atherosclerosis and the complications that go with it is elevated if you are overweight. Even a modest weight loss can help to reduce this risk – dropping 5 to 10 per cent of your total body weight may decrease your risk of heart disease. The location of any excess fat is also important. A waist measurement higher than 35 inches (about 89cm) for a woman or more than 40 inches (about 102cm) for a man is associated with a higher risk of atherosclerosis.
Give Up Smoking (Or Don’t Start)
Smoking is one of the biggest risk factors for the development of atherosclerosis. It is associated with a higher risk of coronary heart disease, peripheral artery disease, stroke, and many other serious health problems. The nicotine in cigarette smoke tightens the blood vessels and makes the heart work harder, and smoking damages the artery walls and encourages the growth of plaque. When addressing lifestyle factors that contribute to atherosclerosis, giving up smoking should be one of the top priorities.
Manage Stress
Finding better ways to deal with stress can help with high blood pressure, a major contributing factor to atherosclerosis. Stress also directly promotes the formation of plaque.
Medications
- For High Cholesterol: the first medications usually prescribed to treat elevated cholesterol are statins. If these don’t work or aren’t right for you, your doctor may prescribe other medications, including ezetimibe, PCSK9 inhibitors, bempedoic acid or omega-3 fatty acids.
- For High Blood Pressure: ACE inhibitors, calcium channel blockers and beta blockers. ACE inhibitors relax the blood vessels by stopping the release of an enzyme created by the body that narrows them. Calcium channel blockers prevent calcium, which makes the arteries and heart contract more forcefully, from entering the cells. Beta-blockers operate by blocking the effects of adrenaline to make the heart beat more slowly and less forcefully, resulting in lower blood pressure. They also open the veins and arteries to allow more blood through.
- For High Blood Sugar: if you have atherosclerosis and diabetes, you may be prescribed metformin, empagliflozin, canagliflozin or liraglutide to help control your blood sugar. In addition to its use for elevated blood sugar, research is increasingly showing that metformin may have some ability to treat atherosclerosis directly.
- To Prevent Blood Clots: Your doctor may prescribe antithrombotic drugs to prevent blood clots. These come in two forms: antiplatelet medications like aspirin, dipyridamole, clopidogrel and ticlopidine, and anticoagulant medications like warfarin or heparin.
- To Treat Blood Clots: If prevention has failed and you have clots due to atherosclerosis, you may be prescribed thrombolytics to break them up. Thrombolytics can break up clots in arteries that may otherwise cause heart attack, stroke, mesenteric ischaemia and other problems, but they must be administered as soon as possible.
- For Angina Pain: for chest pain that can occur with coronary artery disease (angina), a doctor may prescribe nitrates like nitroglycerin, or ranolazine. Beta-blockers, statins, calcium channel blockers and aspirin can also be used to treat angina.

Surgeries
If an atherosclerotic blockage is causing serious problems, your doctor may suggest surgery. Surgeries for atherosclerosis range from less invasive catheter-based procedures to open-heart surgery.
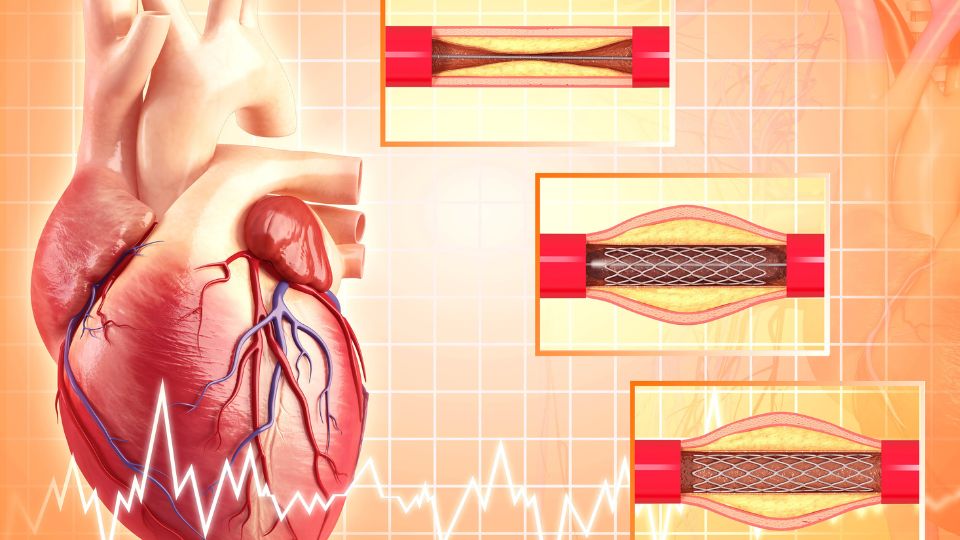
Percutaneous Coronary Intervention (PCI)
The term percutaneous coronary intervention (PCI) is used for any procedure where access to the inside of the body is gained by a needle inserted into the skin rather than by open surgery. This approach is frequently used for atherosclerosis and other issues involving arteries. Types of PCI used to treat narrowing and blockages of the arteries include:
Balloon Angioplasty
In balloon angioplasty, a catheter with a tiny balloon attached to the tip is inserted through an incision in the wrist or groin and fed up to the artery with a blockage. The balloon is then inflated to create more room for blood flow. Often there is also a stent, a tiny mesh tube, over the end of the catheter, and when the balloon is inflated, the stent will be flattened against the arterial walls to ensure the passage remains open. The balloon itself can open up space in the artery, but most patients who get a balloon angioplasty will also have a stent inserted.
Angioplasty With A stent
An angioplasty with a stent is often performed with a balloon, as described above, but not always. There are also self-expanding stents that open inside the arteries with a spring mechanism.
Laser Angioplasty
In a laser angioplasty, a catheter with a laser is sent into the artery. The laser is then used to destroy the blockage.
Rotational Atherectomy
Rotational atherectomy uses a catheter with a rotating device called a rotablator attached to the end. This spins around to pulverise the plaque into pieces smaller than red blood cells. These can then harmlessly be carried away in the bloodstream. Angioplasty and stenting are often used after rotational atherectomy to help prevent the artery from narrowing again.
Open Surgeries
Open surgeries are those where the body is ‘opened’ with an incision made by a scalpel so the surgeon can see the area being operated on.
Endarterectomy
An endarterectomy is an open surgery where an incision is made in the skin to get into the artery from outside the body. This technique is commonly used for blockages of the carotid arteries (carotid endarterectomy) but may also be used in other arteries, including the femoral artery (femoral endarterectomy) or the coronary arteries (coronary endarterectomy).
Transmyocardial Laser Revascularisation
In transmyocardial laser revascularisation (TMR or TMLR), an opening is made in the side of the chest, and tiny channels are made in the outside surface of the heart with a laser to improve blood flow. This technique is often used in patients with advanced heart disease or other problems that make angioplasty or coronary artery bypass grafting too risky.
Coronary Artery Bypass Grafting
Coronary artery bypass grafting (CABG) improves blood flow to the heart by using functioning arteries from the chest or veins from the legs to reroute blood to ‘bypass’ the blocked arteries. This is the most invasive surgery described here. During the procedure, the breastbone must be opened up to expose the heart, and the heart itself may be stopped while a machine performs its functions and keeps you alive. However, there are less invasive versions of CABG where there is no need to cut bone, and the heart can be allowed to keep beating during surgery.

How Can Atherosclerosis Be Prevented?
All of the healthy lifestyle advice that doctors suggest to treat atherosclerosis is also good for preventing its development in the first place:
- Eat a healthy diet.
- Get regular exercise.
- Don’t smoke.
- Keep your stress under control.
In addition to these, you can reduce your risk of atherosclerosis by controlling any health conditions you have which are risk factors, like diabetes, high blood pressure and obesity. Take any prescribed medications, follow your doctor’s advice, get regular checkups, and seek medical advice if there are any changes in your condition.
Can Atherosclerosis Be Reversed?
Clinical trials indicate that atherosclerosis is, to some extent, reversible with a combination of strict healthy lifestyle changes and treatment with cholesterol-lowering medications. For treatment to work best, very high doses of the drugs were needed.
Conclusion
Atherosclerosis can be the first stage of many serious conditions, so it should be taken seriously. However, you have a great degree of control over the health of your arteries. By making healthy lifestyle choices, you can prevent atherosclerosis from progressing, or from beginning in the first place. Even if you’ve already received the news that you have a problem, there are many effective options for treatment.