When you hear the word ‘infection,’ you probably think about bacteria or viruses. And you’d be right – those two families of microorganisms account for the common cold, the flu, COVID-19, strep throat, whooping cough and most kinds of food poisoning. Still, fungal infections make up some of the most common maladies doctors and pharmacists hear about, including athlete’s foot and thrush. Let’s dig into the world of fungal infections, find out the symptoms and treatments for the most common types, and learn about some more serious (and, thankfully, less common) ones.
What Is A Fungal Infection?
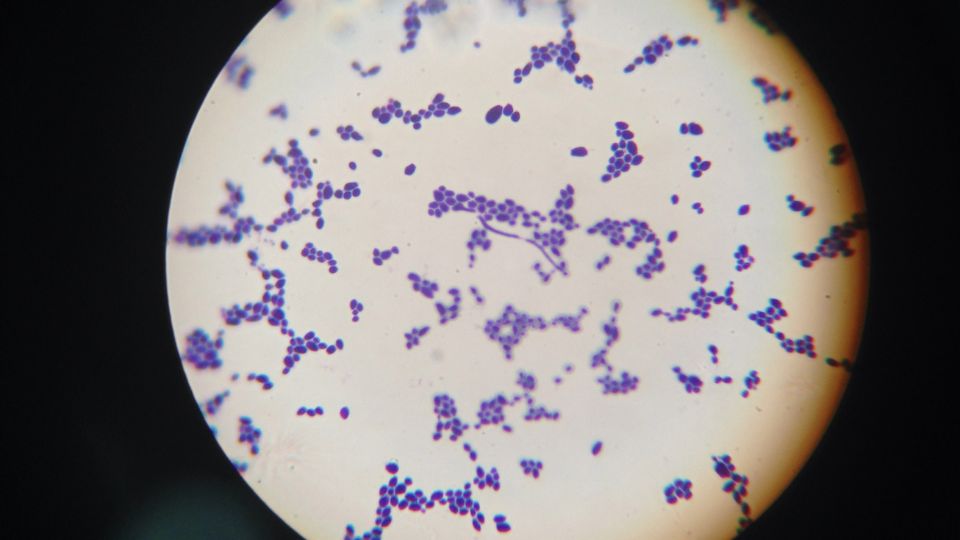
A fungal infection (or a mycosis) is an infection caused by a particular type of microorganism called a fungus (the plural is fungi). These organisms include yeast, mould, and the mushrooms we eat. Humans naturally have billions of fungi, bacteria and other living things on and in our bodies, usually with no ill effects, as part of an ecosystem called a microbiome. Fungal infections occur when the fungi that are naturally present are allowed to grow out of control or when fungi that aren’t usually found on or in you find a home in or on your body and start a colony. Fungi reproduce by releasing spores, which can be picked up by touching or inhaling them, and this is how humans can get infected with fungi that don’t naturally live on us.
Common Types Of Fungus That Can Cause Infection In Humans
Most of the common fungal infections found in humans are caused by three different types of fungi: dermatophytes, Candida and Malassezia.
Dermatophytes
Dermatophytes are a type of fungi that feeds on keratin, the non-living tissue that makes up most of your hair and nails, as well as the outer layer of your skin. They are behind athlete’s foot, jock itch, ringworm and fungal nail infections.

Candida
Candida albicans is a yeast that lives naturally on most people’s bodies without causing problems. It only causes trouble when it is allowed to grow out of control or gets into the bloodstream. Candida causes thrush (or ‘yeast infections’), most commonly on and in the genitals and mouth.
Malassezia
Malassezia is another type of yeast that usually makes a home in people’s bodies without any trouble, but if the microbiome gets out of balance, its populations can surge, resulting in an infection. Malassezia causes Malassezia folliculitis (fungal acne) and is thought to have a role in seborrhoeic dermatitis.

Immunosuppression And Fungal Infections
People whose immune systems are weakened either by health conditions or medications are at a greater risk of getting fungal infections and of experiencing serious complications if they do get fungal infections. This condition is sometimes called being immunocompromised, immune-compromised or immunosuppressed.
Immunosuppression can be caused by health conditions including:
- AIDS or HIV
- Poorly-controlled diabetes
- Cancer
- Malnutrition
Immunosuppression can be caused by taking medications including:
- Corticosteroids
- Biologics and biosimilars
- Chemotherapy drugs
- Organ transplant medications
If any of the above applies to you, and you think you may have any of the fungal conditions described in this article, see your doctor before attempting self-treatment with over-the-counter products.
Athlete’s Foot
Also Called
Tinea pedis
Where Is It
Unsurprisingly, athlete’s foot is found on the feet. But the fungus can spread to other parts of the body.
Type Of Fungus
Dermatophytes
Symptoms
- Itching, burning or stinging sensation on the foot, especially between the toes
- Cracking, peeling, scaling or blistering of the skin
- Discolouration of the skin
- A soft, mushy texture in the affected skin
- Skin layers starting to break down
Diagnosis
- A doctor may diagnose the symptoms just by looking at the skin.
- Skin scrapings may be taken and examined under a microscope.
Treatment
- Over-the-counter topical treatments
- Prescription topical treatments are available for more severe infections that don’t respond to over-the-counter preparations, containing ingredients including clotrimazole, econazole, and ciclopirox
During treatment, keep your feet clean and dry and avoid going into public showers or changerooms barefoot.

Risk Factors
Athlete’s foot is common in athletes, hence the name. The fungus thrives in warm, moist areas like locker rooms and public showers, so athlete’s foot is more likely to be a problem for people who use these facilities more often. In addition, it’s more common in people who wear tight, closed shoes and sweaty socks for too long without changing them.
Is It Contagious?
Yes, athlete’s foot can spread from one person to another, and you catch it from surfaces or items with the fungus on them, like floors or shoes.
Prevention
Keeping your feet clean and dry and wearing sandals in locker rooms and public showers can help to prevent athlete’s foot.
See A Doctor If You Have Suspected Or Diagnosed Athlete’s Foot And:
- The condition doesn’t improve within two weeks of beginning treatment with over-the-counter products
- You have diabetes
- You have trouble with your circulation
Jock Itch
Also Called
Tinea cruris
Where Is It
Jock itch is found on the groin, inner thighs and buttocks.
Type Of Fungus
Dermatophytes
Symptoms
- Redness (on light skin, may be brown or grey on darker skin)
- There may be a circular red rash
- A burning sensation
- Itching
- Flaking skin
- Cracking skin
- A rash that worsens when you exercise
Diagnosis
A doctor will usually be able to recognise jock itch by the visible condition of the skin, but they may also take and test a sample of skin cells to rule out other conditions like psoriasis.
Treatment
It’s frequently possible to control jock itch with over-the-counter antifungal topical products. During treatment, it’s important to keep the area clean and dry and change your clothes daily, especially your underwear.
Risk Factors
Jock itch is most common in men and boys. Being overweight can provide a more hospitable environment for the fungus, as it means there are more folds of skin to give it somewhere warm and moist to live. For the same reasons, having a tendency to sweat a lot, wearing a lot of tight clothes or living in warm, humid climates makes it more likely that you’ll get it. As with any fungal infection, it’s more common in people with compromised immune systems.
Is It Contagious?
Yes, you can get jock itch through close contact with someone with it or their clothing.
Prevention
- Wash your hands regularly.
- Wash and dry the affected area regularly.
- Avoid tight clothing, especially in hot or humid weather.
- If you already have athlete’s foot, get treatment for that because the same fungus causes them, and it can spread from your feet to your groin, causing jock itch.
See A Doctor If:
You suspect you have jock itch, and the problem doesn’t improve after two weeks of treatment with over-the-counter products, the area looks infected, or the rash spreads to other parts of your body.
Ringworm
Also Called
Ringworm is a form of tinea, like athlete’s foot and jock itch. Tinea has different names according to where on the body it appears and how the rash looks: ringworm is the name given to tinea that causes a rash in a circular shape. This is most likely to happen on the body (tinea corporis). Tinea may appear on many other parts of the body, including the hands (tinea manuum), scalp (tinea capitis), face (tinea faciei) and beard (tinea barbae), but in these places, it’s less commonly called ‘ringworm’ and less likely to have the characteristic ring shape. Ringworm is also known as dermatophytosis, after the dermatophyte that causes it.

Type Of Fungus
Ringworm is caused by dermatophytes. It doesn’t involve worms of any kind – it gets its name from the circular shape that the tinea rash often has.Symptoms
Ringworm on the body usually begins as an itchy red rash, forming a circle that gets less red on the inside, creating the ring shape it’s known for. There may be blistering and oozing, and if the infection is on the scalp, there may be bald patches, itching and scaly skin.Diagnosis
Ringworm can be diagnosed with a visual examination by a doctor. The dermatophytes fungus glows under a special light called Wood’s lamp. The doctor may take samples of your skin to be tested and ask whether you’ve been in contact with other people or animals infected with ringworm (ringworm can be transmitted from animals to humans – and vice versa).Treatment
Ringworm can usually be treated with over-the-counter topical antifungal treatments, but if these don’t work, there are stronger antifungals your doctor can prescribe.Risk Factors
Factors that increase your likelihood of getting ringworm include:- Having a weakened immune system
- Using public locker rooms or showers
- Being an athlete (especially one playing contact sports)
- Wearing tight clothes
- Sweating a lot and having close contact with animals
Is It Contagious?
Yes, you can get ringworm through contact with someone who has it (or an animal who has it) or with surfaces it’s on.Prevention
- Keep your skin clean and dry.
- Change your clothes every day (especially socks and underwear).
- Keep your fingernails and toenails short and clean.
- Don’t go barefoot in public showers and locker rooms.
- After you touch an animal, wash your hands with soap and water.
- Shower and change into clean clothes immediately after exercise.
- Don’t share personal items like towels and clothing with someone who is infected.
See A Doctor If:
Get medical help if the rash isn’t responding to home treatment, many patches of skin are affected, or it seems to be spreading. If you think you may have tinea capitis (a fungal infection on the scalp), see a doctor, as this is particularly difficult to treat with over-the-counter products.Yeast Infection
Also Called
‘Yeast infection’ is a common name given to the condition known to doctors as candidiasis, after the fungus that causes it. Another common name for the condition is thrush – depending on the part of the body where it appears, it may be called oral thrush, vaginal thrush or genital thrush (it can also affect males).
Type Of Fungus
Candida albicans
Symptoms
Candida most commonly appears in or around your mouth or on male or female genitals.
| In Vaginal Thrush | In Genital Thrush (Male) | In Oral Thrush |
|
|
|
In vaginal thrush and male genital thrush, there may be no noticeable symptoms.
Diagnosis
For suspected vaginal thrush, a doctor will conduct a pelvic exam and may swab the area for samples. Thrush has symptoms similar to other medical conditions, including sexually transmitted diseases. The doctor may conduct tests to rule out underlying health problems if you have thrush outbreaks a few times per year.
For suspected genital thrush in men, a doctor will examine your genitals and may swab the area for samples and test them.
For suspected oral thrush, a doctor will examine the inside of your mouth, ask about your symptoms and test swabs of skin cells taken from the affected area. If your doctor thinks you may have thrush as far back as your oesophagus (sometimes spelled esophagus), they may send you to get an endoscopy to confirm the diagnosis.
Treatment
The treatment given will depend on what kind of yeast infection it is, where it is, and whether it recurs often.
Vaginal: it’s common to begin treating suspected vaginal thrush with over-the-counter antifungals, including topical creams and pessaries. If this doesn’t work, you should visit a doctor. They are likely to prescribe medications that can be applied topically, given orally as a pill, or administered as a vaginal suppository, with a stronger antifungal component than products you can buy over the counter. If you keep getting thrush, your doctor may prescribe a longer course of treatment.
Male genital thrush: Over-the-counter topical treatments can also be used for male genital thrush. As with vaginal thrush, if treatment with over-the-counter products doesn’t fix the problem, you should see a doctor for stronger treatments. Keeping the area clean and dry during treatment is a good idea to make it harder for the yeast to live there.
Oral thrush: There are over-the-counter antifungal treatments, including oral drops. A doctor can prescribe stronger treatments, including oral medications.
Risk Factors
The risk of all forms of thrush may be increased by having poorly-controlled diabetes, cancer, HIV or other immune-lowering conditions. Use of antibiotics or corticosteroids, a poor diet, skin irritation, stress or hormone imbalances may also make an outbreak more likely.
The risk of oral thrush may be increased by smoking, having a dry mouth or wearing dentures, especially if they don’t fit well.
Is Thrush Contagious?
Not generally, but person-to-person transmission sometimes occurs, especially in people with compromised immune systems.
Prevention
| Vaginal Thrush | Male Genital Thrush | Oral Thrush |
|
|
|
See A Doctor If:
Seek medical help if you know or think you have vaginal thrush, and any of these apply to you, even if you have already seen a doctor about your thrush:
- You think you have thrush and you have a lowered immune system
- Your thrush is resistant to treatment
- You have sores on the skin of your genitals, stomach pain or abnormal vaginal bleeding
- You are pregnant or breastfeeding
- You are diabetic
- You get repeated outbreaks of thrush
- You feel sick or feverish
If you are male and have thrush, see a doctor if:
- You suspect you have thrush and you have a lowered immune system
- Over-the-counter treatments haven’t helped
- You have seen a doctor already, and the treatments they prescribed haven’t helped
- You keep getting thrush
- Your symptoms are severe
If you have oral thrush, see a doctor if:
- You only suspect you have thrush and you have a lowered immune system
- Your sores won’t go away with treatment
- You have difficulty swallowing
Any child with white patches or bleeding sores inside their mouth should be taken to a doctor. If your child is known to have thrush, take them back to the doctor if they are showing signs of dehydration.
Be prepared for the unlikely possibility of a common illness like thrush turning serious by enrolling in an accredited first aid course.
Onychomycosis
Also Called
Tinea unguium, toenail or fingernail fungus, fungal nail infection
Type Of Fungus
Dermatophytes
Symptoms
- A light-coloured spot on the nail
- Nails flaking or crumbling
- Nails becoming thicker or brittle
- Nails lifting off the nail bed
- Scaling (buildup of skin) underneath the nail

Diagnosis
A doctor may take scrapings from an affected nail and examine them under a microscope to rule out conditions with similar symptoms.
Treatment
Treating nail infections can take a long time because nails are made of multiple layers of keratin, and dermatophytes can get between those layers and sometimes even into the matrix, where the nail grows from. Treatments available for fungal nail infections include topical creams and nail polishes that you can get over the counter from your local pharmacy and keep in your first aid cabinet. A doctor may consider prescribing oral antifungal medication, especially if the patient has a lowered immune system.
Risk Factors
You are more likely to have a fungal nail infection if you:
- Have sweaty feet
- Wear closed shoes for extended periods
- Have psoriasis
- Are diabetic
- Have an injury or deformity of the feet, hands or nails
- Have a compromised immune system
- Have poor circulation in your legs
- Have fungal infections of other parts of the body
Is It Contagious?
Yes. A fungal nail infection can be spread from one person to another either by direct contact or touching a surface with which an infected person has been in contact.
Prevention
- Keep your feet clean and dry.
- Keep your toenails short.
- Wear a clean pair of socks every day.
- Wear well-fitting shoes.
- Wear sandals in public bathrooms and changing rooms.
- Don’t share shoes or personal care items like nail clippers.
See A Doctor If:
- The infection isn’t improving with home treatment.
- One of your nails has turned brown or black.
- One of your nails starts lifting off the nail bed.
- One of your nails suddenly hurts.
- You have diabetes, and there is any change in the condition of your feet.
Malassezia Folliculitis
Also Called
Fungal acne, fungal folliculitis, pityrosporum folliculitis
Type Of Fungus
Malassezia Folliculitis is caused by the Malassezia yeast, which lives on the skin without causing problems in most people. Note, like the various kinds of thrush, Malassezia Folliculitis is a yeast infection, but when people use the term ‘yeast infection’, they are usually referring to an infection caused by Candida.
Symptoms
The main symptom of Malassezia Folliculitis is a rash of small, pimple-like red lumps, sometimes with white heads, on the upper back, shoulders and chest. It sometimes also appears on the face; when it does, it will likely be on the forehead. Malassezia Folliculitis is often mistaken for acne and is colloquially known as fungal acne, but real acne is bacterial, not fungal.

Diagnosis
A doctor will examine your skin, possibly under Wood’s lamp, as the Malassezia yeast glows under it. To confirm the diagnosis, they may also take a sample of skin cells and look at them under a microscope. You may also be referred to a dermatologist.
Treatment
Some people with fungal folliculitis have good results treating it themselves using anti-dandruff shampoo with antifungal ingredients as a body wash or applying over-the-counter antifungal creams meant for other conditions. A doctor can prescribe stronger topical or oral antifungal treatments if this doesn’t work.
Risk Factors
- Antibiotics can disrupt the natural balance of microorganisms on the skin, killing both good and bad bacteria and allowing Malassezia yeast to proliferate.
- Teenagers are more likely to get fungal folliculitis because they tend to have oilier skin, and the yeast feeds on oil.
- Men are more likely to get it than women.
- Diabetics are at greater risk.
Is It Contagious?
No, Malassezia folliculitis is not contagious.
Prevention
- Wash regularly with an antifungal cleanser.
- Avoid tight clothes, and try to wear natural, breathable fabrics.
- Wash at least once a day.
- Don’t use oily skincare products.
- Avoid shaving every day if the rash is on a part of the body you shave.
- If you exercise, shower, change into clean clothes afterwards, and wash your sweaty clothes immediately.
- Don’t eat too many carbohydrates or sugary foods as they provide food for the yeast.
See A Doctor If:
- Treatment with over-the-counter products is not helping.
- You have already seen a doctor about your condition, and the treatment they have prescribed is not working.
- You feel sick or have a fever.
Seborrhoeic Dermatitis
Also Called
Seborrhoeic eczema, dandruff (if mild and on the scalp), cradle cap (if on a baby’s head). ‘Seborrhoeic’ may also be spelled ‘seborrheic’.
Type Of Fungus
Seborrhoeic Dermatitis may be caused by the body’s reaction to the Malassezia yeast, the same one that causes Malassezia folliculitis, but doctors are not sure of this.
Symptoms
Seborrhoeic dermatitis is typified by patches of oily, scaly or flaky skin. The scaling may be white or yellowish, and the skin underneath may be red. It only appears on the seborrhoeic areas of the skin (those that produce sebum, or oil), most commonly the scalp – dandruff is a mild form of seborrhoeic dermatitis. Cradle cap can cause scaling on babies’ scalps.
Diagnosis
A doctor will usually diagnose seborrhoeic dermatitis by examining your skin, but they may take a biopsy to rule out conditions with similar symptoms, especially if your condition doesn’t respond to treatment.

Treatment
Antifungal shampoos can effectively treat seborrhoeic dermatitis on the scalp in adults. For cradle cap affecting babies, the scales can be softened with warm water and olive oil or baby shampoo and then carefully removed with a cotton bud or a soft brush. For seborrhoeic dermatitis on other areas of the skin, treatment will usually consist of over-the-counter antifungals, or if those don’t work, stronger antifungals prescribed by a doctor. Corticosteroids can also be prescribed to treat itching and redness.
Risk Factors
- Being male
- Having oily skin
- Stress
- Fatigue
- A family history of psoriasis
- Living in a cold region
- Changing seasons
- Having an immune disorder
- Having a mental illness, including depression
Is It Contagious?
No, seborrhoeic dermatitis is not contagious.
Prevention
You can’t prevent seborrhoeic dermatitis, as its exact causes are unknown. But people who have it usually notice that specific things trigger their flare-ups, and you can reduce the likelihood of further outbreaks by avoiding these triggers.
Common Triggers For Seborrhoeic Dermatitis Include:
Stress
Find ways to minimise and manage stress in your life.
Cold, Dry Weather Conditions
You may be able to reduce flare-ups on your scalp by wearing a warm hat in winter.
Hot Water
Make sure your showers or baths aren’t too hot, as this can dry out your skin, especially in cold weather.
Harsh Detergents And Chemicals
Wear gloves when handling harsh chemicals like those used for cleaning, and only use gentle, alcohol-free personal care products on your skin.
Sweat
Sweat aggravates seborrhoeic dermatitis, so wash and change into clean clothes immediately after exercise.
See A Doctor If:
You don’t see any improvement in your condition with treatment, your symptoms suddenly worsen, or the problem interferes with your life.
Serious Fungal Infections
So far, we’ve looked at more superficial fungal infections, those that affect only the skin, nails and areas of mucosal tissue that go a little way into the body, like the mouth or vagina. But fungal infections become serious when they penetrate deeper into the body, sometimes causing life-threatening problems. This usually only happens in people whose immune systems are weakened in some way.
Fungal Sinusitis
Fungal sinusitis is an inflammation caused by an infection in the paranasal sinuses, empty spaces in the front of the skull. It’s caused by the inhalation of mould or yeast spores. Fungal sinusitis may be the least dangerous of the more invasive fungal infections discussed in this section, but in people without strong immune systems, it can be serious, even spreading to the brain. Such people are also more likely to get fungal sinusitis in the first place. Treatment will involve oral antifungals and may include surgery in more severe cases.
Symptoms Of Fungal Sinusitis:
- Fever
- Nasal congestion
- Nasal discharge
- Headaches, especially around the eyes, forehead or cheeks
- Changes in vision
- Protruding eyes
- Changes in sense of smell
- Changes in mental state
- Face pain, swelling or numbness – any pain may be on one side, and the area may be tender to the touch
- Changes in skin colour
Fungal Pneumonia
Inhaling fungal spores can cause fungal pneumonia (fungal lung infection). Pneumonia can have a variety of causes, and bacterial and viral pneumonia are each more common than fungal pneumonia. Fungal pneumonia is mostly caused by inhaling fungal spores, but the fungus can also spread to the lungs through the bloodstream from an infection elsewhere in the body. Fungi species that cause pneumonia include those found outdoors in specific regions, including Coccidioides, Histoplasma, Cryptococcus neoformans and Blastomyces. Pneumonia can also sometimes be caused by Candida in immune-compromised people.

Symptoms Of Fungal Pneumonia
- Coughing, possibly coughing up blood
- Shortness of breath
- Fatigue
- Fever
- Joint and muscle pain
- Chest pain
- Headaches
- Night sweats (more common in infections with Blastomyces or Coccidioides)
- Chills
Fungal Eye Infection
Fungal eye infections are caused either by fungal spores from outside the body (sometimes via contact lenses) or by a fungal infection carried to the eye from elsewhere in the body by the bloodstream. Treatment depends on how deep in the eye the infection is and can include:
- Antifungal drops
- Oral or intravenous antifungal medications
- Injections into the eye
- Surgery in severe cases
As with all fungal infections, immunocompromised people are at a higher risk of both getting an infection in the first place and experiencing complications as a result.
Symptoms Of A Fungal Eye Infection
- Pain or redness
- Discharge
- Blurred vision
- Tearing
- Sensitivity to light
Candidaemia And Invasive Candidiasis
Invasive candidiasis is a serious Candida infection where the fungus reaches deeper into the body, infecting the organs, eyes, bones or blood – candidaemia is the name for a Candida infection of the bloodstream (sometimes also spelled candidemia). It usually happens in environments like hospitals, and the infection is often caused by medical interventions that involve opening the skin, like intravenous catheters or abdominal surgeries. Like other fungal infections, invasive candidiasis is more likely to occur in people with compromised immune systems.
Symptoms Of Candidaemia Or Invasive Candidiasis
Invasive candidiasis can cause different symptoms depending on where the infection is: any of the more serious fungal infections discussed in this section could indicate the presence of invasive candidiasis, and they each have their own symptoms. The following are some more general symptoms of invasive candidiasis:
- Abdominal pain
- Fever and chills (especially if, after a bacterial infection is suspected, they’re treated with antibiotics and show no improvement)
- Fatigue
- Muscle aches
- A rash
- Low blood pressure
- Trouble breathing
- A rapid heart rate
- Multiple organ failure
Fungal Meningitis And Fungal Encephalitis
Meningitis is a condition where the membranes surrounding the brain and spinal cord (called the meninges) become inflamed due to an infection. Encephalitis is the same thing but in the brain itself. Both are more likely to be caused by a bacterial or viral infection than a fungal one, but fungal meningitis and encephalitis sometimes occur. Meningitis will often spread to the brain, causing encephalitis and vice versa. Fungal meningitis and fungal encephalitis generally begin when a fungal infection elsewhere in the body spreads to the central nervous system. They are both treated with high doses of antifungal medication.
Symptoms Of Fungal Meningitis Or Encephalitis
- Headache
- Fever
- Neck pain or stiffness
- Nausea
- Vomiting
- Sensitivity to light
- Confusion
See a doctor immediately if you think you have the symptoms of one of these serious fungal infections.

What Are The General Risk Factors For Fungal Infections?
Anyone can get fungal infections, but you may be more vulnerable if one or more of the conditions below applies to you.
Weakened Immunity
As discussed earlier, anything that weakens the immune system makes it easier for fungal infections to take hold. This includes health conditions like cancer, HIV and diabetes that isn’t controlled well enough, as well as some medications used for cancer, autoimmune diseases, and preventing the rejection of transplanted organs.
Antibiotic Use
Fungal infections often pop up just after the sufferer has been treated with antibiotics for a bacterial infection. Antibiotics don’t harm fungi but kill both bad and good bacteria. This throws off the balance of the microbiome and allows fungi populations to explode without competition from bacteria, leading to fungal infections.
Living In Damp Conditions
Whether it’s environmental conditions like humid weather or damp rooms, or the microclimate created on your body by wearing sweaty workout gear for too long, moisture and warmth increase your risk of fungal infection because they provide the environment that fungi need to grow.
Poor Blood Circulation
For any infection to heal, the area needs to be supplied with infection-killing white blood cells. If your blood circulation isn’t the best, these cells may not make it to the site of the infection quickly enough to stop it in the early stages.
Menopause
In women, hormonal changes after menopause decrease the acidity of the vagina, which can make vaginal thrush more likely.
Injuries To The Skin
Cuts and scratches to the skin provide an entry point for fungi to get a bit deeper into tissue and potentially create a more serious infection. Whenever you have a graze, wash it with soap and water immediately, dry it properly and cover it with a sticking plaster or clean bandage.
Living In Or Travelling To Specific Areas
Some more serious fungal infections like coccidioidomycosis (Valley Fever), Cryptococcus gattii infection and paracoccidioidomycosis are more common in certain parts of the world. Unfortunately, it’s difficult to advise about avoiding these, as you catch them by breathing in spores in the air. If you are planning travel, you should read about any potential health risks in the area, especially if you are immune-compromised.
How Can Fungal Infections Be Prevented?
- Wash your body every day and dry it properly, paying particular attention to any folds of skin.
- Wash your hands often, especially after touching animals or other people.
- Don’t share towels, razors and other personal care items with others.
- Wear shoes in locker rooms, community showers, and swimming pools.
- If you are immune compromised, as well as the points above, consider also using an air filter and avoiding plants and flowers, but ask your doctor for specific advice.
Summary
There are many kinds of fungal infections. Most of them are harmless, but they can be a nuisance – they may be hard to treat, or you may have repeated outbreaks. You can help yourself by following the steps above to prevent fungal infections to at least make it more difficult for large colonies of fungi to make a home on you. Unfortunately, it’s common for minor fungal infections to pop up more than once. But if they keep recurring, see a doctor to rule out any underlying conditions. There are some things that should be handled by a medical professional. But it’s a good idea to prepare as best you can for medical problems by enrolling in a first aid course.


