Fatty liver is mostly a lifestyle-related condition that is becoming increasingly common in developed countries as the average diet becomes less healthy and the average person more sedentary. But fatty liver often has no symptoms, and many people live with a fatty liver with no apparent ill effects. So why does it matter if someone has fatty liver? Because it can be a valuable warning sign before serious health conditions develop. A diagnosis of fatty liver disease is a chance to implement some healthy lifestyle changes and prevent worse health problems before they begin.
What Is Fatty Liver Disease?
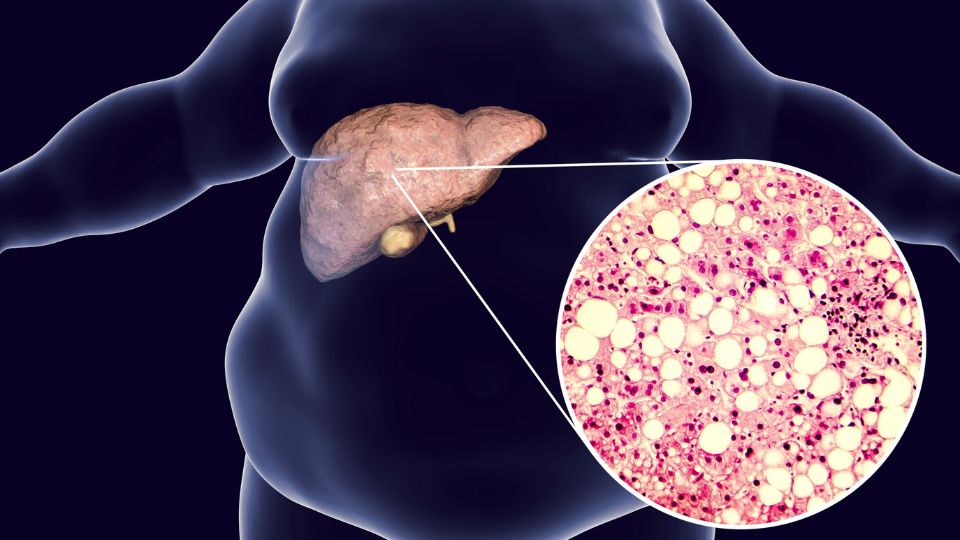
Fatty liver disease (hepatic steatosis) is a condition where extra fat is stored inside the cells of the liver, specifically when the liver accumulates an amount of fat that is 5 to 10 percent of its total weight.
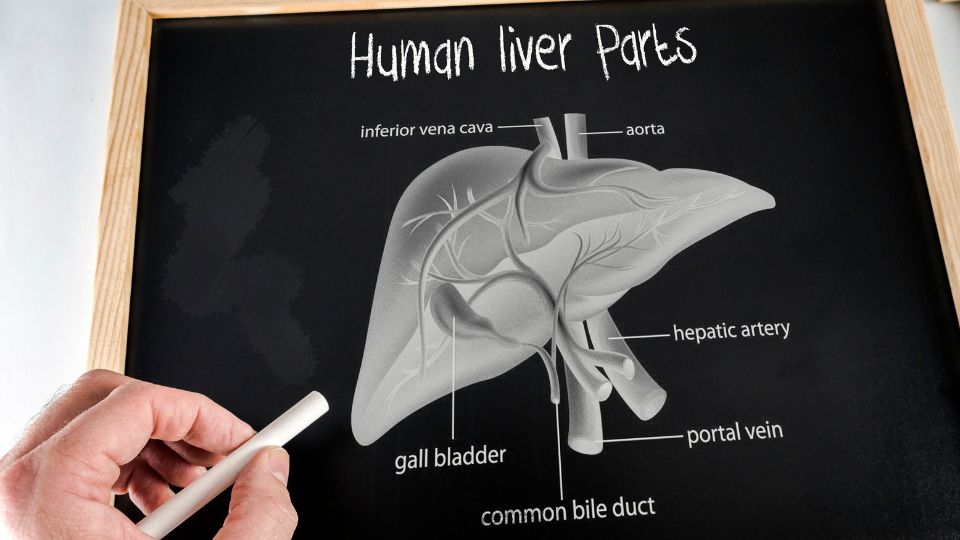
What Does The Liver Do?
The liver is the largest organ in the body and one of the most important. It has many functions, but one of the main ones is processing waste products. The liver has an amazing capacity to regenerate itself as long as it remains healthy. The liver filters waste from the blood and carries it away on a substance it secretes called bile. Bile is also used to digest food, especially fatty food, and is stored in a pouch called the gallbladder for this purpose.
Functions Of The Liver
- Filtering wastes, including medications and bacteria
- Digesting and absorbing dietary fats to use as energy
- Making proteins, including those needed for blood coagulation, iron storage and the transport of vitamins and enzymes around the body
- Storing iron and other vitamins and minerals
- Storing and releasing glucose
- Dealing with wastes from the processing of proteins: the liver transforms toxic ammonia created by the digestion of amino acids into urea that leaves the body through urine
- Regulating hormones
Types Of Fatty Liver Disease
Fatty liver disease can be divided into two main types: one that is caused by long-term excessive alcohol use and one that isn’t. A third type can occur during pregnancy, but this is rare and is usually considered a separate disorder.
Non-Alcoholic Fatty Liver Disease
Non-alcoholic fatty liver disease (NAFLD) is a fatty liver disease that isn’t caused by alcohol use. It is also known as Metabolic (dysfunction) associated fatty liver disease, or MAFLD. NAFLD can be further divided into two subtypes, non-alcoholic fatty liver and non-alcoholic steatohepatitis.
Non-Alcoholic Fatty Liver
Non-alcoholic fatty liver (NAFL) is a type of non-alcoholic fatty liver disease (NAFLD) where there is fat in the liver but no inflammation. NAFL is also called simple fatty liver or simple steatosis. Notice it’s NAFL without the D on the end – NAFLD is an umbrella term which can refer to both NAFL and NASH
Non-Alcoholic Steatohepatitis
Non-alcoholic steatohepatitis (NASH) is a type of non-alcoholic fatty liver disease where there is fat in the liver and also inflammation. NASH can be thought of as either a type of NAFLD or a worsening in the condition of NAFL, but not all cases of NAFL develop inflammation and become NASH. Steatohepatitis is not related to the infectious forms of hepatitis caused by viruses.
How Common Is NAFLD?
NAFLD affects almost one-third of the Australian population, with similar rates in Europe and the US.
Alcoholic Fatty Liver Disease
Alcoholic fatty liver disease (AFLD), also known as alcohol-related liver disease (ARLD) or just alcoholic liver disease (ALD), is a fatty liver disease caused by long-term heavy drinking. It is possible to have both NAFLD and AFLD simultaneously if you have risk factors for NAFLD and drink in excess. Like Non-alcoholic fatty liver disease, AFLD can be divided into two subtypes based on the presence or absence of inflammation: alcoholic fatty liver or alcoholic hepatitis.

Alcoholic Fatty Liver
Alcoholic fatty liver without inflammation is the first stage of alcoholic liver disease. It can appear even after only a few days of heavy drinking, but the damage is reversible at this stage, and the liver should heal itself if the drinking stops for two weeks.
Alcoholic Hepatitis
When alcoholic liver disease progresses to a point where there is both fat and inflammation in the liver, this is called alcoholic hepatitis. Not every person who drinks heavily will develop alcoholic hepatitis, and as with alcoholic fatty liver, the damage is likely to heal on its own if drinking stops. However, alcoholic hepatitis can be fatal if it is severe. Alcoholic hepatitis is not related to viral hepatitis.
Acute Fatty Liver Of Pregnancy
Acute fatty liver of pregnancy is a rare but serious complication of pregnancy, usually occurring in the late third trimester, which can threaten the life of the mother and baby if the condition is not quickly diagnosed and first aid given. The causes are unknown, and the only treatment is to deliver the baby as soon as possible. After this, most patients make a complete recovery with medical care.

What Causes Fatty Liver Disease?
The cause of non-alcoholic fatty liver disease is unknown. However, there are risk factors associated with a higher likelihood of developing it, and these are mostly lifestyle-related. Like heart disease, NAFLD is more common in adults but is becoming more common in children due to the increasing incidence of childhood obesity. It is because of increasing rates of obesity and type 2 diabetes that NAFLD continues to increase worldwide.
Non Alcoholic Fatty Liver disease
Your chances of developing NAFLD are increased if you have any of these health conditions:
- Being overweight or obese, especially having fat around your midsection (central obesity)
- Having insulin resistance or type 2 diabetes
- Your blood cholesterol levels, specifically having high LDL cholesterol, low HDL cholesterol or high cholesterol overall
- Having high blood pressure
NAFLD also occurs occasionally in people who have:
- Reactions to medications, including steroids, chemotherapy drugs, or HIV medications
- Haemochromatosis a condition where the body absorbs too much iron and becomes overloaded
- Chronic hepatitis B
- Chronic hepatitis C
- Polycystic ovary syndrome (PCOS)
- Hypothyroidism
- Sleep apnoea
Fatty Liver And Gallbladder Removal
Increasing evidence indicates that having a gallbladder removal operation (a cholecystectomy) is a risk factor for the development of NAFLD, and that NAFLD is a risk factor for developing gallstones.

Acute Fatty Liver Of Pregnancy
Acute fatty liver in pregnancy is rare, affecting only about five in 100,000 pregnancies. The following factors are associated with an increased risk of getting it.
- Being pregnant with a boy
- Having a multiple pregnancy
- Being pregnant for the first time
- Being thin
Alcoholic Fatty Liver Disease
AFLD is caused by heavy drinking.
What Are The Symptoms Of Fatty Liver Disease?
NAFLD often doesn’t cause any symptoms in its own right unless it progresses to more advanced forms of liver disease, but people who have NAFLD may experience the following:
- Fatigue
- Weight loss
- Loss of appetite
- Abdominal pain, especially in the upper right part of the abdomen

What Are The Possible Complications Of Fatty Liver Disease?
Although the following conditions are listed as complications of a fatty liver, they can also be understood as developments along a continuum – liver disease is often described as occurring in stages. Fatty liver is an early warning of possible trouble, but most people with NAFLD will not develop liver damage, especially if the lifestyle issues that led to fatty liver are addressed.
Steatohepatitis
As well as a form of non-alcoholic fatty liver disease, steatohepatitis can also be thought of as a more advanced stage of NAFLD where there is not just fat in the liver but inflammation and cell damage of the liver tissue. If it occurs with NAFLD, it’s called non-alcoholic steatohepatitis (NASH), and if it occurs with AFLD, it’s called alcoholic steatohepatitis (ASH, or just alcoholic hepatitis). Not all people with fatty liver will develop steatohepatitis, and doctors are not sure why this is. It is usually possible to reverse NASH with healthy lifestyle changes and to reverse the damage from alcoholic hepatitis if you stop drinking for good.
Fibrosis
Fibrosis or scarring occurs in the liver tissue as the liver attempts to heal the inflammation of steatohepatitis. This is the first stage of liver scarring, and the condition is often still reversible at this point with lifestyle changes. Even when fatty liver progresses to some degree of fibrosis, there aren’t always symptoms.
Cirrhosis
An advanced form of liver disease where a considerable amount of healthy tissue is replaced by fibrosis and liver function is impaired – in the later stages of the condition, the liver can be quite scarred and shrunken. Cirrhosis can be life-threatening, and a liver transplant may be needed. Cirrhosis develops in around 10-25% of alcoholics, but it is not just something that affects alcoholics: it can occur with either AFLD or NAFLD. It is possible but unlikely that the damage to the liver can be reversed at this point.
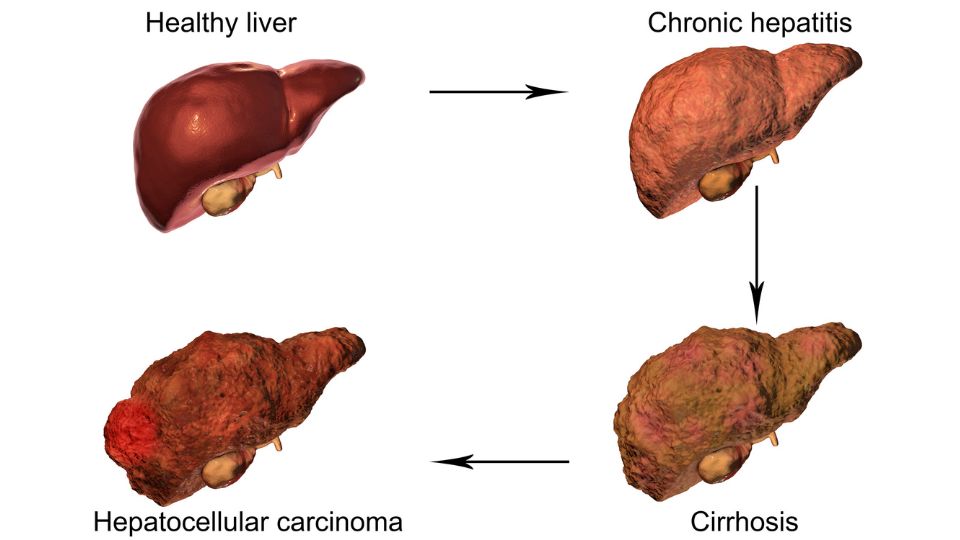
Liver Failure
Cirrhosis can eventually lead to chronic liver failure, also called end-stage liver disease, a condition where the liver gradually ceases to function. Treatment of chronic liver failure includes all the lifestyle changes recommended for earlier stages of liver disease (chronic liver failure is also called end-stage liver disease). The aim here is to save whatever part of the liver is still functioning. A liver transplant may eventually be needed.
Liver Cancer
Cirrhosis can lead to liver cancer. In fact, The majority of people who have liver cancer have cirrhosis. The most common kind of primary liver cancer (as opposed to cancer that spreads to the liver from elsewhere in the body) is hepatocellular carcinoma.
Hepatic Encephalopathy
Hepatic encephalopathy is a complication that can occur in advanced liver disease, where brain function deteriorates because the liver can’t fulfil its normal function of filtering toxic substances. These build up in the blood and reach the brain. It is also called portosystemic encephalopathy (PSE). Hepatic encephalopathy is often temporary and treatable but can become less treatable as the liver disease becomes more severe.
How Is Fatty Liver Disease Diagnosed?
Diagnosis of fatty liver disease will involve a combination of the tests below. If there is fat in the liver but no damage, there is NAFL (or AFL if alcohol is the cause). If there is fat, some inflammation, and cell damage, the diagnosis will be NASH (or ASH if alcohol is the cause).
Interview And Medical History
The doctor is likely to ask about your medical history, including how much alcohol you drink, what medications you take, and whether you have any of the health conditions that are risk factors for fatty liver disease.
Physical Exam
The doctor may press on your abdomen to determine whether your liver is enlarged or painful and listen to it with a stethoscope. They will also be alert for whether your skin or the whites of your eyes are yellow – this is jaundice, a possible sign of cirrhosis.

Blood Tests
Fatty liver is often picked up during routine blood tests that include indicators of liver function, among other levels to be checked. Blood tests to check for liver problems are likely to include a group of tests called a liver function test or liver panel. These are tests to find elevated levels of certain enzymes and proteins, which can indicate If this is found, the doctor may order other tests to rule out the possibility of issues like viral forms of hepatitis. More advanced liver disease can’t be diagnosed with blood tests alone, but doctors can use them to estimate levels of scarring and decide on further testing.
Imaging Studies
The following imaging tests can be used to help diagnose NAFLD:
Ultrasound
During an ultrasound, harmless sound waves are projected through your body using a handheld device called a transducer, creating images of your liver on a screen. A liver ultrasound can spot fatty liver, other structural abnormalities like scarring or enlargement, and inflammation. Liver ultrasounds are a useful indicator of possible liver disease, but they are not definitive. Doctors may order more tests if you are suspected of having liver disease beyond the level of NAFLD. Like blood tests, ultrasound scans are a way that fat in the liver is often inadvertently spotted during an examination related to another issue.
Magnetic Resonance Imaging
A magnetic resonance imaging (MRI) scan uses a powerful magnet and radio waves to generate a picture of your liver. The magnet temporarily moves the water molecules in your body around, and the radio waves use these to create cross-sectional images of the inside of your body. These cross-sections can even be stacked to generate a three-dimensional image. This is possible because the process involves moving you into a tunnel-shaped machine where the scanner moves around your body in a circle. Sometimes a contrast dye is administered intravenously to create a clearer picture. One advantage of an MRI is that it does not use radiation, so it may be used if doctors need more frequent images. An MRI can be used to determine a good place to take a biopsy from. An MRI is better at showing inflammation and problems with soft tissues.

A patient undergoing an MRI scan
Computed Tomography Scan
Like an MRI, a computed tomography (CT) scan can produce three-dimensional images of the inside of your body by moving it into a circular machine with a rotating scanner, but instead of just magnets, it uses radiation in the form of x-rays. The use of contrast dye is also an option with a CT scan. An advantage of CT scans is that the machine your body moves through is more open in construction than an MRI machine (more like going through a donut than going into a tunnel), so many people who find an MRI scan claustrophobic don’t mind CT scans as much. A CT scan is better for showing bone and joint problems, some organ problems and blood clots.

A patient undergoing a CT scan
Elastography
An elastography is an imaging test that evaluates how stiff your liver is to gauge whether there is any fibrosis. A doctor may choose to do this test if you are known or suspected to have any inflammation or damage to the liver or if you have any signs of cirrhosis. Elastography can be done with ultrasound (elastography ultrasound) or with a magnetic resonance machine (magnetic resonance elastography or MRE.
Liver Biopsy
A liver biopsy is the only way to be sure that someone has NASH and the only way to be sure that it’s fatty liver disease causing tissue damage. The doctor removes a small piece of tissue from the liver so a pathologist can examine it with a microscope for signs of inflammation and damage. A liver biopsy does not necessarily have to involve open surgery: it’s often possible to get a sample of liver tissue using a fine needle. Because of the relative invasiveness of the procedure and the risks, doctors are more likely to recommend a biopsy if they believe the condition of the liver has advanced to the point of inflammation and advanced fibrosis, not just where NAFLD alone is suspected.

A doctor performing a liver biopsy using ultrasound as a guide
Can Fatty Liver Be Reversed?
Much of the time, but not always, simple fatty liver can be reversed with lifestyle changes. These can include weight loss, lowering cholesterol, and managing underlying conditions contributing to fatty liver, like hypothyroidism and diabetes.
Can Fatty Liver Disease Kill You?
Fatty liver disease on its own can’t kill you – there is no such thing as first aid for a fatty liver. However, fatty liver disease develops because of unhealthy lifestyle choices. It should be taken as a warning sign of future health problems that can develop if changes aren’t made. A fatty liver indicates that your overall health is not what it should be. It may increase the risk of atherosclerosis and other forms of cardiovascular disease, including heart attack and stroke. Cardiovascular disease is one the most common causes of death in people with NAFLD, so it should be taken as a wake-up call.
Can Fatty Liver Disease Be Prevented?
Some people are more disposed to get fatty liver than others, but it is largely preventable by following the same lifestyle advice doctors recommend for the treatment of the disease once you have it: a healthy diet, regular exercise and maintaining a healthy weight.
See Lifestyle Changes To Manage Fatty Liver Disease and Diet For Fatty Liver Disease below.
What Treatments Are There For Fatty Liver Disease?
The main treatment for fatty liver disease is the implementation of healthy lifestyle changes.
Medications
There are no specific medications for NAFLD, but your treatment may involve taking prescribed medications for any conditions you have that may be contributing to your fatty liver, like diabetes or high cholesterol.
Lifestyle Changes To Manage Fatty Liver Disease
Making changes to your lifestyle can improve and even reverse fatty liver disease. The recent push to change the name of NAFLD to metabolic associated fatty liver disease is in recognition of the connection between non-alcoholic fatty liver and metabolic dysfunction that is largely a result of lifestyle. The following lifestyle changes can improve and even reverse fatty liver disease, provided the liver damage hasn’t progressed too far.
- Drink little to no alcohol (this helps even if your fatty liver is not caused by alcohol use – people with alcoholic fatty liver disease should seek help to abstain from alcohol completely)
- Lose weight (losing 10% of your body weight is very beneficial, but even losing 3 to 5% is good)
- Get regular exercise
- Control your blood sugar levels, and if you have diabetes, follow your doctor’s instructions to manage it
- Control your cholesterol levels
- Give up smoking
- Eat a healthy diet

Diet For Fatty Liver Disease
|
Eat More |
Eat Less |
|
|
Questions To Ask Your Doctor If You Have Been Diagnosed With Fatty Liver
- What has caused my fatty liver?
- Do I have inflammation or cirrhosis in my liver? Am I at risk of developing more serious forms of liver disease?
- Can I reverse my liver damage? If so, how long will it take?
- Should I be taking any medications for my cholesterol levels?
- Are there any medications I should stop taking?
- What other foods or activities should I avoid?
- Should I lose weight? If so, what would be a healthy weight for me?
- Can I get any support for losing weight, improving my diet or reducing my alcohol intake? (if relevant)
Summary
If you’ve made it this far, you’ve seen that while fatty liver disease usually causes no symptoms of its own, it’s a condition that should be taken seriously. Firstly, in some people, fatty liver can progress to steatohepatitis, or fatty liver with inflammation. Once this happens, there is a risk of scarring and damage as the liver tries to deal with this inflammation, which means more serious forms of liver disease. Secondly, even if you have a fatty liver and inflammation never develops, the excess fat means you have an unhealthy lifestyle and are vulnerable to other serious health problems like diabetes and cardiovascular disease. You can help prevent these conditions by making the recommended healthy lifestyle changes. You can also prepare for the possibility of more severe health conditions in yourself or others by enrolling in an accredited first aid course.