It’s often said that men tend to neglect health problems until they become serious and are less likely to see a doctor than women, and there’s some truth to both of these statements. More men than women die from virtually every illness both sexes can experience. Even in diseases that affect more women than men, men will sometimes experience worse outcomes once diagnosed, possibly due to the tendency to seek help only once the illness has progressed. The good news is simple lifestyle changes can prevent many of the most common health conditions men suffer. Keep reading to learn about some of the most common health conditions in men and what you can do to avoid them.
Cardiovascular Disease In Men
According to data from the Australian Bureau of Statistics, ischaemic heart disease, a form of cardiovascular disease also known as coronary heart disease or coronary artery disease, was the leading killer of men in Australia in 2021.
What Is Cardiovascular Disease?
Cardiovascular disease (or heart disease) is a disease affecting the heart and blood vessels.
What Are The 5 Most Common Cardiovascular Diseases?
It’s difficult to say what the most ‘common’ cardiovascular diseases are because this is complicated by the relationships between different forms of cardiovascular disease. For example, coronary heart disease can lead to heart failure. Using Australian Institute of Health and Welfare data from 2018 to 2019, we can look at the number of hospitalisations for each form of cardiovascular disease and rank them from most to least number of people admitted to hospital with the disease in question as a principal diagnosis. By doing this, we can get a top five of the most common cardiovascular diseases affecting Australian men.

What Are The 5 Most Common Cardiovascular Diseases In Men?
1. Coronary Heart Disease
Coronary heart disease, also known as ischaemic heart disease or coronary artery disease, is a chronic condition caused by blockages to the arteries that provide blood to the heart. Coronary artery disease can cause a heart attack or cardiac arrest.
2. Heart Failure And Cardiomyopathy
- Heart failure (or congestive heart failure) is a chronic condition that occurs when the heart has become so weak it can no longer pump blood effectively, and pressure builds up in the blood vessels of the lungs, making them leak fluid.
- The term cardiomyopathy covers a series of diseases that affect the heart muscle and constrict the heart’s ability to pump blood. Although the AIHW does not differentiate between heart failure and cardiomyopathy and puts them jointly at number two, cardiomyopathy is a heart muscle disease that affects the heart’s ability to pump blood around the body adequately and can be a cause of heart failure. Cardiomyopathy can cause cardiac arrest.
3. Atrial Fibrillation
Atrial fibrillation is a particular type of irregular heartbeat caused by the fibrillation, or quivering, of the heart’s upper chambers. Atrial fibrillation is manageable but can lead to heart failure, stroke and other complications if left untreated.
4. Stroke
A stroke is a disruption of the blood supply to the brain. This can be either due to a blood clot or an accumulation of plaque blocking a blood vessel (ischaemic stroke) or when a blood vessel in the brain ruptures (haemorrhagic stroke).
5. Peripheral Arterial Disease
Peripheral arterial disease is a lack of blood flow to body parts other than the heart or brain due to the narrowing or blockage of blood vessels. It can cause serious consequences like organ damage or loss of limbs, fingers or toes.
The number of people hospitalised with these types of heart disease is higher for men than women. In fact, out of the eight major causes of cardiovascular disease hospitalisations listed in AIHW Table 3, the only one which has a greater number of hospitalisations for women than men is hypertensive disease.

What Are The Signs Of Cardiovascular Disease In Men?
Although men are more likely than women to experience chest pain as a symptom of heart attack (only about half of women who have heart attacks get chest pain), the first signs of heart disease can be more annoying than painful. Any of the following symptoms could indicate a heart attack, so if you experience them, see a doctor immediately. Call an ambulance if you think you or someone else is having a heart attack.
Warning Signs Of Heart Disease
- Having trouble catching your breath after moderate exercise like walking up stairs
- Discomfort or pressure in your chest that goes for thirty minutes or more
- Pain in your jaw, neck or upper torso with no obvious explanation
- Changes in the speed of your heartbeat, whether it’s slower or faster than normal
- An irregular heartbeat
- Fainting or feelings of dizziness
- Pain in your chest
- Pain, tingling, numbness, coldness, weakness or swelling in your arms or legs
- Severe fatigue
A dry cough, fever and rashes on the skin can indicate heart disease caused by an infection in the heart.
What Is A Cardiac Arrest?
A cardiac arrest, also known as a sudden cardiac arrest, is a malfunction in the heart’s electrical signals that causes an irregular pumping rhythm arrhythmia (most commonly ventricular fibrillation), making the heart stop. A person experiencing cardiac arrest will rapidly lose consciousness. This lack of blood supply can result in permanent brain damage or sudden death if allowed to continue for only a few minutes.
What Is A Heart Attack?
A heart attack happens when there is a blockage of one of the arteries supplying blood to the heart. A heart attack can be sudden and painful or have gradual mild symptoms like those listed under early signs of heart disease. A heart attack can even have no symptoms at all. Whatever the symptoms, a heart attack can cause serious damage to the heart and even death.
How Can You Tell If Someone Is Having A Cardiac Arrest Or Heart Attack?
Generally, someone having a cardiac arrest will be unconscious and not breathing normally, while someone having a heart attack will still be conscious and breathing but feeling pain or discomfort. However, the difference can only be determined for sure by a medical professional. Furthermore, a heart attack can lead to cardiac arrest, so it should be treated extremely seriously.
If you think someone is having a cardiac arrest or a heart attack, call emergency services for an ambulance (000 in Australia). If the person is unconscious, begin administering cardiopulmonary resuscitation (CPR). A professional first aid course can teach you how to perform CPR properly and needn’t take more than a day.
How Can You Tell If Someone Is Having A Stroke?
Stroke is the fourth most common cause of heart disease hospitalisations for men. Stroke has certain outward signs, and if you see them in yourself or someone else, you should seek immediate medical attention. The longer a stroke goes untreated, the greater the risk of brain damage or death.
The FAST Signs Of Stroke
The Stroke Foundation recommends learning the following common signs of stroke. You can memorise them using the acronym ‘FAST’.
Face: Look at the person’s face. Is it drooping, especially the mouth?
Arms: Ask them to try lifting both their arms. Do they have any trouble with this? Are they unable to lift both arms to the same height?
Speech: Is the person slurring their words? Do they have trouble understanding you?
Time: If you see any of these symptoms, don’t waste time calling for an ambulance.
What To Do If You Think Someone Is Having A Stroke
If you think someone is having a stroke, call 000 if you are in Australia and ask for an ambulance immediately. While you wait for it to arrive, you can do the following:
- If they are conscious, help them to lie on their side with their head slightly elevated.
- Don’t give them any food or drink.
- If they are wearing any clothing that might restrict their breathing, loosen it.
- Check whether they are breathing. If not, start performing CPR.
When you call an ambulance, the operator will guide you through what you need to do. However, you can become more prepared for any emergency where you have to perform CPR or give any other first aid by taking part in an accredited first aid course.
What Causes Stroke?
A stroke happens when the blood supply to the brain is disrupted, either when plaque or a blood clot blocks a blood vessel (ischaemic stroke) or when a blood vessel bursts (haemorrhagic stroke).
What Causes Cardiovascular Disease?
There are some risk factors for cardiovascular disease that you can’t control, like having a family history of it, getting older, or having a congenital heart condition. But two of the major causes of heart disease are atherosclerosis and high blood pressure, and you can either prevent or mitigate these with the lifestyle decisions you make.
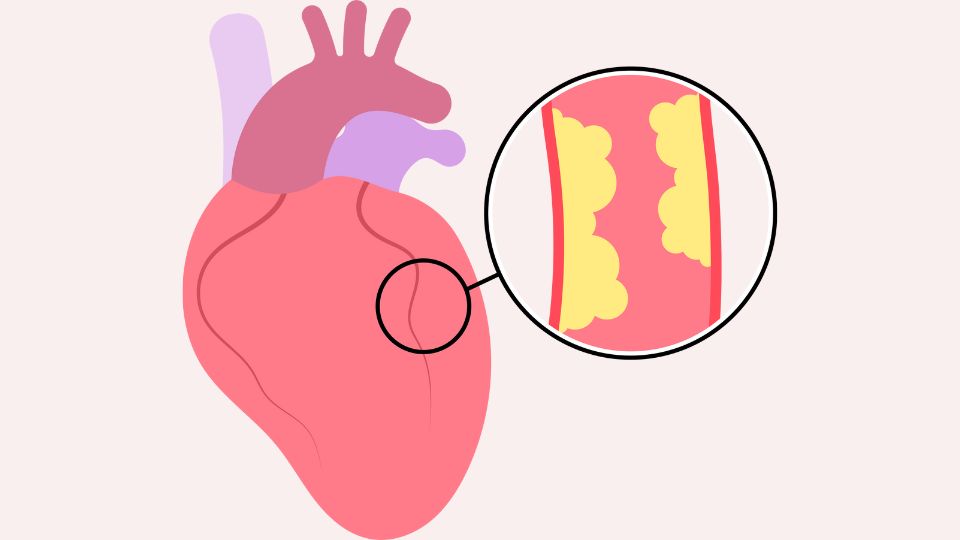
Atherosclerosis
Coronary heart disease is the most common form of heart disease, and its immediate cause is atherosclerosis. This is a gradual process where plaque builds up inside the arteries that provide blood to the heart, making it harder for the blood to get through.
Long-Term High Blood Pressure
Another important contributing factor to coronary heart disease is long-term high blood pressure. High blood pressure can harm your arteries by making them stiffer, which, like atherosclerosis, restricts blood flow to the heart. High blood pressure is also the most significant risk factor for stroke.

Lifestyle Factors
You can significantly reduce your risk of atherosclerosis, high blood pressure, and heart disease by controlling your lifestyle-related risk factors. You can go a long way to good heart health by eating a healthy diet, exercising, not smoking, maintaining a healthy weight, reducing stress, getting enough sleep and keeping up with your health screenings.
For more detail, see How Can Cardiovascular Disease Be Prevented, below.
How Is Cardiovascular Disease Diagnosed?
The first indication that you may have heart disease will probably be one of the Early Signs Of Heart Disease listed above, or if you’re really unlucky, a more serious episode like a cardiac arrest. Once heart disease is on the radar as a possibility, doctors can use a range of different techniques to diagnose it.
Common Ways Doctors Diagnose Heart Disease
Blood Tests
When your heart is damaged (for example, by a heart attack), it releases substances into the blood that can be detected in a blood test. Before heart damage occurs, doctors can also perform blood tests evaluating your cholesterol levels to determine your risk of atherosclerosis.

Electrocardiogram
A doctor can read the electrical activity of your heart and see whether it is beating as it should with a test called an electrocardiogram (also called an ECG or EKG) by attaching electrodes to your body with sticky pads and using a machine to create a recording of the information.

Exercise Stress test
This is an electrocardiogram done while you’re exercising to examine the function of your heart during exercise.

Echocardiogram
An echocardiogram uses a type of x-ray called an ultrasound to create a picture of your heart and help the doctor determine whether anything is wrong. The picture is picked up with a probe that’s either held against your chest or down your throat (the latter can provide better pictures as the probe doesn’t have to go through bone).

Nuclear Cardiac Stress Test
In this test, a doctor injects you with a small amount of radioactive material to track how well your blood can flow through your arteries and heart. A special imaging machine is used to pick up the pictures.

Coronary Angiogram
In a coronary angiogram, a tiny tube is put into one of your arteries and moved inwards until it reaches your heart. It then injects a dye that enables the coronary arteries to be picked up on an x-ray.

Magnetic Resonance Imaging
Also called an MRI, magnetic resonance imaging creates still images or video of your heart using radio waves and magnets.

Coronary Computed Tomography Angiogram
A computerised tomography scan (also called a CT scan or CAT scan) is a high-powered x-ray machine that can make images of the inside of your body in a cross-section format. A coronary computed tomography angiogram is what it’s called when images are taken with this technique to diagnose coronary artery disease.

How Can Cardiovascular Disease Be Treated?
If you’re diagnosed with cardiovascular disease, your treatment will depend on what kind it is and how severe it is. Treatment for cardiovascular disease may include:
Lifestyle Changes
Your doctor may suggest changes like improving your diet, increasing the amount of exercise you get and quitting smoking.
Medication
You may be prescribed medications to address your heart condition. These could include blood thinners, statins to lower cholesterol, or medications that promote blood flow and reduce blood pressure.
Surgeries
Surgeries to address cardiovascular disease can range from procedures considered ‘minimally invasive‘, like inserting stents to hold arteries open, all the way up to heart transplants.
Cardiac Rehabilitation
You can think of cardiac rehabilitation as one step up from the kind of lifestyle changes recommended above: cardiac rehabilitation is a supervised program to improve the strength of your heart, including lifestyle advice and treatment from a team of healthcare professionals in areas like diet, exercise and stress management.
Monitoring
Regardless of what other interventions you have for heart disease, your doctor will want to keep an eye on your heart health in the future.
How Can Cardiovascular Disease Be Prevented?
Reducing the risk of cardiovascular disease is within their control for most men: more than 80% of coronary artery disease, the most common kind of heart disease, can be prevented by following a healthy lifestyle.
How To Reduce Your Risk Of Heart Disease
1. Don’t Smoke
Smoking lowers the amount of oxygen in the blood, making the heart work harder to get enough oxygenated blood to the brain and the rest of the body. This increases blood pressure. Smoking also causes atherosclerosis, damaging the blood vessels and heart.
2. Get Between 30 And 60 Minutes Of Exercise Every Day
Exercise increases the strength of the heart muscle and reduces the risk of conditions that harm the heart, like diabetes, high blood pressure and high cholesterol.
3. Improve Your Diet
A diet that’s good for the heart has:
MORE | LESS |
Fruits And Vegetables | Salt |
Legumes | Sugar |
Lean Meat | Processed Carbohydrates |
Fish | Alcohol |
Dairy Foods With Low Fat Or No Fat | Saturated Fats |
Whole Grains | Trans Fats |
Healthy Fats Like Olive Oil |
4. Stay At A Healthy Weight
As well as maintaining a body mass index lower than 25, keeping your waist circumference lower than 101.6 cm or 40 inches decreases the risk of heart disease for men.
5. Get Enough Sleep
Not getting enough sleep increases your risk of high blood pressure, heart disease, diabetes, obesity and depression.
6. Control Stress
Stress can cause high blood pressure, which can lead to heart disease.
7. Keep An Eye On Your Health With Regular Screenings
Get your doctor to regularly test you for high blood pressure and cholesterol and periodically screen you for diabetes. These are all risk factors for cardiovascular disease.
Male Risk Factors For Cardiovascular Disease
Keep an eye on these male health problems, as they may be an early indication of developing heart problems.
Erectile Dysfunction
Problems with getting or maintaining an erection can be an early warning sign of coronary heart disease. The inability of the blood vessels to open properly (endothelial dysfunction) is one of the earliest stages of coronary heart disease, which is often seen first in the penis.
Low Testosterone
Low testosterone levels in men are associated with a higher risk of heart disease, so it’s a good idea to watch for symptoms that your levels are not where they should be, like a lowered sex drive, loss of muscle mass, irritability, fatigue, and depression. Erectile dysfunction can be a sign of low testosterone and a possible indicator of endothelial dysfunction.
Diabetes In Men
Diabetes was the seventh largest underlying cause of death for men in 2020, according to the Australian Institute of Health and Welfare National Mortality Database supplementary data tables (Table S3.1). Men seem to be more vulnerable to developing diabetes than women: it takes men less weight gain than women to be at a higher risk of diabetes, according to a study by the University of Glasgow. More men than women also have undiagnosed diabetes, possibly because men are less likely to see a doctor about health concerns.

What Is Diabetes?
Diabetes is a health condition in which the body either cannot use or make insulin, or both. Insulin is the hormone that enables your body to use blood sugar for energy. Diabetes causes excess glucose in the blood, which can cause serious health complications. There are two forms of diabetes (excluding gestational diabetes, which only affects women), type 1 and type 2.
Type 1 Diabetes
Type 1 diabetes is an auto-immune disease where the body’s immune system destroys its insulin-producing cells, making the person with diabetes unable to produce their own insulin. There are genes connected to a high risk of developing type 1 diabetes, but unlike type 2, it’s not known to be associated with any modifiable lifestyle factors, and it usually appears early in life. There is effective treatment available but no cure, and the cause is unknown.
Type 1 Diabetes In Men
Type 1 diabetes is more common in males than females. According to Australian government figures, for males, it’s 14 in 100,000, and for females, it’s 10.
Type 2 Diabetes
In Type 2 diabetes, the body develops a resistance to the effects of insulin and eventually loses its ability to make its own insulin. Unlike type 1 diabetes, whether you get type 2 diabetes is largely within your control, and it can be avoided with lifestyle choices.
Type 2 Diabetes In Men
Overall, type 2 diabetes is slightly higher in men than in women in Australia, according to AIHW statistics, and it’s higher for men within every individual age category past the age of 45.
Early Signs Of Diabetes In Men
Early signs of diabetes are the same in both men and women. Some common early signs of diabetes are:
- Urinating frequently
- Fatigue
- Blurry vision
- Weight loss with no obvious explanation
- Numbness or tingling in the feet and hands
How Does Diabetes Affect The Male Body?
Erectile Dysfunction
Although any man can be affected by erectile dysfunction (the inability to get or keep an erection), it’s particularly likely in men with diabetes. A meta-analysis of 145 studies in 2017 found that more than half of men with diabetes experienced erectile dysfunction. This is because diabetes damages the nerves and blood vessels.
Retrograde Ejaculation
Retrograde ejaculation is a problem that can occur with ejaculation, where the semen enters the bladder instead of coming out through the penis. It can happen in diabetic men due to nerve damage from diabetes (diabetic neuropathy).
Low Testosterone
Low testosterone is common in men with both type 1 and type 2 diabetes because of the high concentration of glucose that tends to be in their blood. High blood glucose makes it difficult for the body to make the right amount of luteinising hormone, a substance necessary for testosterone production. Low testosterone in men can have symptoms including low sex drive, erectile dysfunction, low sperm count, trouble concentrating, depression, sleep problems, a decrease in the size and strength of muscles, and bone loss.
Both Men And Women Can Experience The Following Effects Of Diabetes:
Cardiovascular Disease
People with diabetes tend to have high cholesterol levels and blood pressure. Either can increase the risk of heart attack, stroke and other diseases affecting the heart and blood vessels.
Eye Problems
Diabetes increases your risk of eye problems, including retinopathy, macular oedema, cataracts and glaucoma.
Kidney Disease
Diabetes can cause harm to the small blood vessels of the kidneys, resulting in kidney disease. It’s important to screen for this, as kidney disease has no discernible symptoms until the damage is underway.
Nerve Damage
In addition to the erectile dysfunction discussed above, the nerve damage that results from poorly-controlled diabetes can affect the nerves that control the functions of body organs and the nerves that affect feeling and movement anywhere in the body.
Foot Problems
Diabetes can cause neuropathy and damage to the blood vessels of the feet. This can slow normal healing, make infection more likely, induce ulcers and deform the structure of the foot. Perhaps most dangerously, neuropathy in the feet reduces their sensation, so any injuries or problems you have there could get badly out of control before you notice anything is wrong.
Problems With The Teeth And Gums
If your diabetes isn’t controlled, you’re at a higher risk of tooth decay and gum infections because of damage to the small blood vessels in your gums.
Infection
The high blood glucose levels that result from poorly-managed diabetes impede the action of the white blood cells that fight infection, which weakens your immune system.
Thyroid Problems
Diabetes increases your risk of thyroid disease, both hypothyroidism (underactive thyroid) and hyperthyroidism (overactive thyroid).
Incontinence
Neuropathy from diabetes can affect the muscles of your bladder and bowels, making it more difficult to sense when they are full or control their actions.
Even if you have already been diagnosed with diabetes, none of these effects is inevitable. You can greatly reduce the risk of all long-term effects of diabetes by managing your condition and keeping your blood sugar under control.
Diabetes Treatments
The treatment you need for diabetes will vary depending on what kind of diabetes you have, but it may include the following:
- Making adjustments to your diet: this may mean eating less of the kind of carbohydrates that cause a rapid rise in blood sugar.
- Increasing the amount of exercise you get: exercise increases your body’s sensitivity to insulin and helps you control your blood sugar levels
- Controlling your weight:
- If you have type 2 diabetes, being overweight makes it harder to control your blood glucose levels. Suppose you’re a type 2 diabetic and you’re also obese. In that case, there’s a possibility losing weight could put your diabetes into remission (a sustained return to normal blood glucose levels without the use of medication).
- If you have type 1 diabetes, losing weight could mean a reduction in the amount of insulin you need to take and will certainly reduce your risk of complications.
- Taking medications: some of the most common medications that may be prescribed to a diabetic include insulin (a certainty for type 1 diabetics), alpha-glucosidase inhibitors to help your body break down starches and sugars, and biguanides to control the amount of glucose your liver makes.
- Giving up smoking: in diabetics who smoke, quitting improves the ability of insulin to control their blood sugar.
Blood Sugar Problems
Diabetes treatments are about keeping blood sugar at a healthy level, but it can be difficult to get the balance right. Diabetics can experience problems with blood sugar that is too low (hypoglycaemia) or too high (hyperglycaemia). Either can be serious if left untreated, resulting in coma and even death.
Hypoglycaemia | Hyperglycaemia | |
Causes |
|
|
Symptoms |
|
|
Treatment |
|
|
See a doctor immediately or call emergency services if you or someone else experience these symptoms |
|
|
How To Reduce Your Risk Of Diabetes
As stated, you have some control over whether you get type 2 diabetes if you try to reduce your lifestyle risk factors. You may notice many of the things that are good for treating diabetes are also good for preventing it.
Four Ways To Reduce Your Risk Of Type 2 Diabetes:
- If you’re overweight or obese (especially if you’re carrying excess fat around your waist), take steps to lose weight.
- Get 150 minutes per week of exercise at a moderate intensity.
- Improve your diet, especially taking care to reduce your intake of sugary drinks, reduce your portion sizes, and eat more fibre, healthy grains and protein.
- If you smoke, give up.
Cancer In Men

What Are The 5 Most Common Cancers In Males?
According to the AIHW’s report Cancer in Australia 2021, the most commonly diagnosed forms of cancer in men were:
Type/Site Of Cancer | Number Of Cases |
Prostate cancer | 18,110 |
Melanoma of the skin | 9,869 |
Colorectal cancer | 8,247 |
Lung cancer | 7,460 |
Non-Hodgkin lymphoma | 3,694 |
As we can see, prostate cancer was not only the most commonly-diagnosed cancer in men in 2021 but there were almost twice as many cases of prostate cancer diagnosed than there were of the second most commonly diagnosed cancer in men, melanoma.
What Is The Life Expectancy Of A Man With Prostate Cancer?
This depends on how early the cancer is discovered. Per the AIHW figures (via the Prostate Cancer Foundation of Australia), the relative survival rate after five years is 100% for a man in Australia with prostate cancer diagnosed at Stage I. If the cancer is diagnosed at Stage IV, the survival rate is only 36.4%, which shows how important regular prostate cancer screenings are.
Interestingly, although prostate cancer was the most commonly-diagnosed cancer in men for that year, it was not the leading cause of cancer deaths in men: that was lung cancer.

How Do Men Get Prostate Cancer?
The exact cause of prostate cancer isn’t known, but some factors increase your risk of getting it. Unfortunately, many of them are things that are out of your control.
Known Risk Factors For Prostate Cancer
- Age: prostate cancer is extremely rare in men under 40. The average age for a man diagnosed with prostate cancer in Australia in 2022 was 69
- Family history: men with a family history of prostate cancer or cancers of the breast or ovary are more likely to be diagnosed with prostate cancer
- Race: there is a greater risk of prostate cancer in black men for reasons that are not understood
- Obesity: obese men appear to be at a higher risk of dying from prostate cancer.
What Are The 5 Warning Signs Of Prostate Cancer?
There are more than five signs of prostate cancer, but those below are possibly the five most common ones:
- Blood in your urine or semen
- Needing to urinate frequently, especially at night
- Experiencing erectile dysfunction that’s new for you
- Burning or pain when you urinate or ejaculate
- Problems with urinating: trouble stopping or starting urination, or having a weak or interrupted stream when you do urinate
Some other signs of prostate cancer include: problems ejaculating, unexplained weight loss, unexplained pain in the prostate area when you sit down, swelling in the lower body, pain in your bones and bowel or urinary habits that are not normal for you.
Many, if not most, of these symptoms could have explanations other than prostate cancer (for example, many of the top five can occur as a result of benign prostate gland enlargement) but if you experience any of them, see your doctor straight away. Remember, the earlier prostate cancer is detected, the greater the chances of treating it successfully.
Is Prostate Cancer Curable?
Prostate cancer is treatable and can go away forever, but doctors usually use the term ‘in remission‘ rather than ‘cured’ when cancer has been successfully treated. More specifically, if the cancer has stopped growing, it’s ‘in partial remission’, and if it’s disappeared altogether, it’s ‘in complete remission’, and remissions can last a lifetime for some people, meaning their cancer was effectively ‘cured’. As said above, the prospects for a man still being alive five years after a prostate diagnosis are excellent as long as it’s caught early.
How Is Prostate Cancer Treated?
Treatment for prostate cancer depends on factors including your age, how fit you are, whether you have a slow-growing or aggressive type of prostate cancer, what your doctor thinks will help, and what you want. Below is a rough guide to what your doctor may propose depending on whether the cancer is contained (limited to the prostate) or has spread.
If Your Prostate Cancer Is Contained, Treatments May Include | If Your Prostate Cancer Has Spread, Treatments May Include |
Watchful WaitingDoctors monitor your prostate cancer in a minimally intrusive way and don’t give treatment unless symptoms change. | Watchful WaitingWatchful waiting may be an option in advance cancer when the priority is to control symptoms of the cancer rather than cure it . |
Active SurveillanceDoctors monitor your prostate cancer closely. Active surveillance may involve prostate-specific antigen blood tests (PSA tests), digital rectal exams (DREs), prostate biopsies and imaging tests. | Radiation TherapyRadiation therapy is an option for prostate cancer. that has spread. This can be either with the aim of slowing the growth of cancer to prolong your life, or to treat the symptoms of your cancer. |
SurgeryThis could be removal of the prostate (radical prostatectomy) or transurethral resection of the prostate (TURP). | ChemotherapyThis is when drugs are administered, usually through an IV (intravenous) line into your vein, to slow the growth of cancer and shrink it. |
Radiation TherapyWhere the cancer is destroyed with x-ray beams aimed directly at it. | Targeted TherapiesProstate cancer in some men may be treatable with drugs called PARP inhibitors, which can keep cancer cells from repairing themselves and induce their deaths. This kind of therapy is only useful for tumours with a particular kind of mutation, which your doctor can test you for. |
Internal Radiation Therapy (Brachytherapy)A doctor puts radioactive material directly into the prostate . | Clinical TrialsYou may be able to get experimental treatments by taking part in clinical trials if they are available near you. |

Can Prostate Cancer Be Prevented?
Just as we can only point to risk factors for prostate cancer rather than definite causes, we can only talk of things that reduce your risk of prostate cancer, not things that prevent it. But the good news is that all the things statistically associated with a lower risk of prostate cancer are good for you in general, too.
How To Reduce Your Risk Of Prostate Cancer
- Eat less saturated fats and trans fats, and include omega-3 fatty acids in your diet
- Eat more fruits and vegetables
- Drink more green tea
- Avoid overcooked, charred meat
- Stay at a healthy weight
- Exercise regularly
- Give up smoking
- Cut down on drinking
- Get enough vitamin D
- Maintain your sex life
Cardiopulmonary Disease In Men
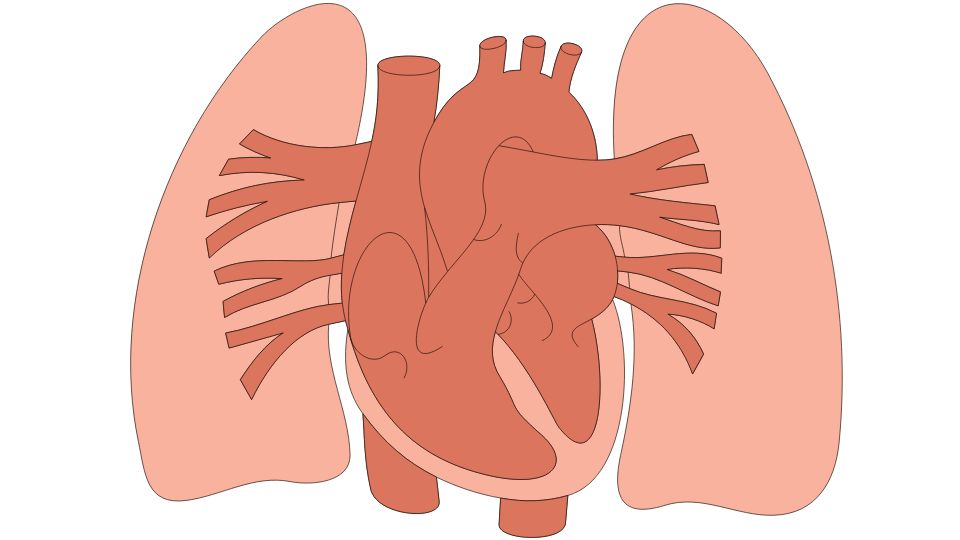
What Is Cardiopulmonary Disease?
A cardiopulmonary disease is one that affects both the heart and lungs. To break this term down, ‘cardio’ refers to things that affect the heart and ‘pulmonary’ refers to things that affect the lungs. There is an extremely close relationship between the heart and lungs, so heart disease can often affect the lungs and vice versa. For example, chronic obstructive pulmonary disorder (COPD), a disease of the lungs, can cause pulmonary hypertension (high blood pressure in the arteries of the lungs and the right side of the heart), which can ultimately result in heart failure.
What Are Some Cardiopulmonary Diseases?
Examples of common cardiopulmonary diseases include pulmonary hypertension, pulmonary embolism and pulmonary oedema. See below for an in-depth discussion of each.
What Causes Cardiopulmonary Disease?
Cardiovascular disease is the most common cause of cardiopulmonary diseases. Still, they have a variety of other causes and risk factors including genetic predispositions and problems with other organs (especially the lungs, of course).
How Is Cardiopulmonary Disease Diagnosed?
Depending on the disease in question, diagnosing cardiopulmonary disease may include such techniques as blood tests, coronary angiograms, echocardiograms, electrocardiograms, x-rays, ultrasounds, pulse oximetry, MRIs, CT scans or ventilation-perfusion (V/Q) scans.
What Are The 3 Common Symptoms Throughout The Cardiopulmonary Disorders?
The three most common symptoms across the cardiopulmonary disorders described here are:
- Breathing problems like shortness of breath or wheezing
- Feelings of fatigue, lightheadedness or faintness
- Cyanosis (bluish discolouration of the skin, especially around the lips, fingers and toes).
Pulmonary Hypertension:
What Is It?
Pulmonary hypertension is when the arteries connecting the heart to the lungs experience high blood pressure.

What Are The Causes?
The immediate cause of pulmonary hypertension is the narrowing of the pulmonary arteries that supply blood to the lungs. This narrowing can have its own underlying causes, including genetic disorders, heart disease, connective tissue disease, blood clots in the lungs, congenital heart disease, lung diseases, liver diseases, chronic kidney failure and HIV/AIDS.
Effects On Men
Although pulmonary hypertension is diagnosed more often in women than men, men seem to respond less well to treatment than women do.
How Is It Diagnosed?
Pulmonary hypertension has symptoms similar to other heart and lung conditions so diagnosis can take a while. After an initial examination by a doctor, the diagnostic process may include an echocardiogram to take pictures of the pulmonary arteries and catheterisation of the pulmonary arteries and heart to measure the blood pressure.
What Are The Symptoms?
- Shortness of breath
- Tiredness
- Lightheadedness or dizziness
- Faintness
- Chest pain
- Heart palpitations
- Swelling (oedema) of the feet, legs or abdomen
- Cyanosis (bluish discolouration of the skin)
What Are The Long And Short-Term Effects?
Short term: the walls of the pulmonary arteries can become stiffer and thicker, which makes it harder for them to expand to let blood through. In the long term, this can cause heart failure.
How Is It Treated?
Treatment for pulmonary hypertension can include either inhaled or injected medicine, diuretics to treat swelling in the legs and feet and oxygen therapy.
How Can Pulmonary Hypertension Be Prevented?
Pulmonary hypertension has many risk factors that are not (or not entirely) within the control of the individual, but you can reduce your risk by:
- Getting enough exercise
- Eating a diet that’s good for your heart, that is, one that’s low in processed foods, salt and saturated fat and high in fruits and vegetables and whole grains
- Not smoking
- Taking any medications your doctor prescribes for blood pressure and other conditions
Pulmonary Embolism:
What Is It?
A pulmonary embolism is a blood clot obstructing the blood flow in one of the arteries of the lungs. The clot usually begins elsewhere, most commonly the leg, and makes its way to the lung.

What Are The Causes?
The immediate cause of a pulmonary embolism is the blood clot obstructing the pulmonary artery. Underlying risk factors for getting such clots include a family history of blood clots, heart disease, cancer, undergoing surgery, inherited disorders that make blood more likely to clot and experiencing severe symptoms of COVID-19.
What Are The Symptoms?
Symptoms include:
- Shortness of breath
- Chest pain
- Fainting
- Lightheadedness or dizziness
- Fever
- Excessive sweating
- Pain or swelling in the legs
- Cyanosis (bluish discolouration of the skin)
How Is It Diagnosed?
The process of diagnosing a pulmonary embolism may include: blood tests to detect elevated levels of clot-dissolving substances made by the body and levels of oxygen and carbon dioxide, chest x-rays, ultrasound, CT pulmonary angiography to generate a cross-sectional image of the pulmonary arteries, a ventilation-perfusion (V/Q) scan where a radioactive substance is injected to track blood flow, a pulmonary angiogram or an MRI.
How is it treated?
Treatment for pulmonary embolism can include medications like anticoagulants (blood thinners ) or fibrinolytic therapy (intravenous medicines to break down the clots), or surgical procedures like placing a small metal device called a vena cava filter in the vein leading from the legs to the right side of the heart or removing the clot with a catheter thin enough to be threaded through the blood vessels.
Effects On Men
Studies have found that pulmonary embolism affects a similar amount of men and women overall, but women are more likely to get it between the ages of 20 and 40, and men are more likely to get it after 60. Pulmonary embolism is also more likely to recur in men.
What Are The Long And Short-Term Effects?
The reduced blood flow that results from a pulmonary embolism can result in tissue damage to the lungs, and low oxygen levels that can cause damage to other organs. A pulmonary embolism can be fatal.
How Can Pulmonary Embolism Be Prevented?
You can minimise your risk of blood clots by:
- Exercising regularly
- Not smoking
- Maintaining a healthy weight
- Eating a healthy diet with lots of fruits, vegetables and whole grains and low in salt
- Staying hydrated
- Not sitting still for too long: get up and move around every hour or so, or at least change position if you can’t get up because you’re travelling
- Don’t sit with your legs crossed
- Avoid tight-fitting clothes
Pulmonary Oedema:
What Is It?
Pulmonary oedema (or edema if you’re American) is a condition where fluid builds up in the air sacs (alveoli) of the lungs and stops them from dispersing oxygen into the blood and ridding the body of carbon dioxide effectively.

What Are The Causes?
Pulmonary oedema is frequently caused by congestive heart failure. It can also be caused by other heart conditions, including heart attack, damaged heart valves, arrhythmias and cardiomyopathy. Additional causes include sudden high blood pressure, pneumonia, sepsis, and lung damage resulting from infection.
There are two categories of pulmonary oedema: cardiogenic pulmonary oedema, which is caused by heart problems, and noncardiogenic pulmonary oedema, which is not caused by heart problems.
What Are The Symptoms?
Pulmonary oedema can be either acute (coming on suddenly) or chronic (coming on gradually). Acute pulmonary oedema can be fatal if left untreated; chronic pulmonary oedema is less dangerous.
Symptoms Of Acute Pulmonary Oedema Can Include:
- Lightheadedness or dizziness
- Feeling weak
- Feelings of anxiety or restlessness
- Cyanosis (bluish discolouration of the skin)
- Cold, clammy skin
- A feeling as though you’re drowning, which may get worse when you lie down
- Heart palpitations
- Breathing problems, including gasping, wheezing or shortness of breath
- Coughing up frothy spit, which may have blood in it
If you have any of the above symptoms, call emergency services for an ambulance at once.
Symptoms of chronic pulmonary oedema can include:
- Rapid weight gain
- Swelling of the legs and feet
- Wheezing
- Tiredness
- Finding it hard to breathe when lying down
- Waking in the night and finding it hard to breathe, and experiencing relief if you sit upright
How Is It Diagnosed?
Tests used to diagnose pulmonary oedema include:
- A chest x-ray
- Pulse oximetry to determine the level of oxygen in the blood
- Various other blood tests, including tests to evaluate kidney and thyroid function
- A coronary angiogram
- An electrocardiogram to monitor the strength and regularity of the heartbeat by attaching electrodes to the body and linking them up to a screen that displays results
- Echocardiogram generating pictures of the beating heart using ultrasound
- An ultrasound of the lungs to show fluid buildup
How Is It Treated?
Usually, the first step in treating pulmonary oedema is administering oxygen to raise the patient’s blood oxygen levels and relieve their symptoms. Depending on what caused the condition, other treatments may include diuretics to help the body shed excess fluid and medications for high or low blood pressure, strengthening the heart muscle, alleviating pressure on the heart, or controlling the heartbeat.
Effects On Men
Pulmonary oedema affects more men than women.
What Are The Long And Short-Term Effects?
As pulmonary oedema continues, it can have effects on the body including breathing problems or lower body swelling (if the patient wasn’t experiencing those already), pulmonary hypertension, pleural effusion (a buildup of fluid in the membranes around the lungs–remember, pulmonary oedema is a buildup of fluid in the air sacs inside the lungs) and swelling and congestion in the liver.
How Can Pulmonary Oedema Be Prevented?
You can help to prevent cardiogenic pulmonary oedema, the most common form of pulmonary oedema, by taking care of your general heart health. This includes:
- Exercising regularly
- Staying at a healthy weight
- Eating lots of fruits, vegetables and whole grains
- Reducing salt in your diet
Conclusion
When you see the grimmer outlook for men across many health conditions, it’s easy to feel discouraged. But remember that most of the conditions described in this article can be prevented, alleviated or controlled by taking steps toward a healthier lifestyle. If you want to go even further toward taking control of your health and being ready to help others, continue your education by enrolling in an accredited first aid course.


